The new tool developed by Norris Cotton Cancer Center and Dartmouth College is the first to use fluorescence to distinguish cancerous tissue from normal tissue in low-grade tumors.
A new probe developed collaboratively at Norris Cotton Cancer Center and Dartmouth College’s Thayer School of Engineering uses an innovative fluorescence-reading technology to help brain surgeons distinguish cancerous tissue from normal tissue. The probe tool, now already in use at the Cancer Center for brain surgery, may one day be used for surgeries for a variety of cancers.
Performing surgery to remove a brain tumor requires surgeons to walk a very fine line. If they leave tumor tissue behind, the tumor is likely to regrow; if they cut out too much normal tissue, they could cause permanent brain damage.
“Primary brain tumors look just like brain tissue,” says Keith Paulsen, PhD, a professor of biomedical engineering at Thayer School of Engineering and a member of the Cancer Imaging and Radiobiology Research Program at Norris Cotton Cancer Center. “But if you look at them under a particular kind of light, they look much different.”
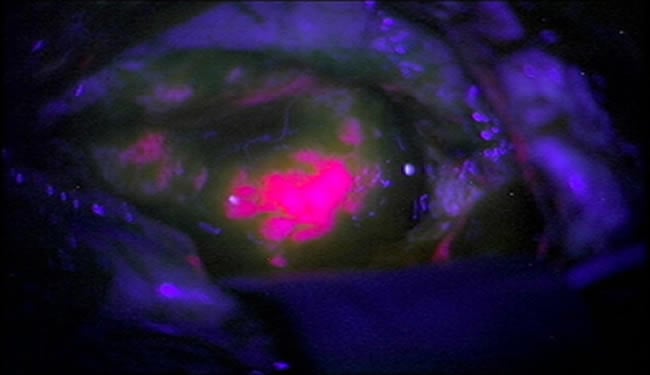
To improve their ability to differentiate between tumor cells and healthy tissue, surgeons can have patients take an oral dose of the chemical 5-aminolevulinic acid (ALA). An enzyme metabolizes ALA, producing the fluorescent protein protoporphyrin IX (PpIX). Tumor cells have a higher metabolic rate than normal cells, so they accumulate more PpIX – and therefore fluoresce, or “glow,” when exposed to blue light.
But this method was thought to be not sensitive enough to highlight brain tumors that are less metabolically active, like low-grade gliomas. To address this problem, MD-PhD student Pablo Valdes, PhD, and his research mentors-David Roberts, MD, the chief of neurosurgery at Dartmouth-Hitchcock Medical Center, and Dr. Paulsen-used a probe (which they helped develop) that combines violet-blue and white light to simultaneously analyze both the concentration of PpIX and four other tumor biomarkers: PpIX breakdown products, oxygen saturation, hemoglobin concentration, and irregularity of cell shape and size. The probe reads how light travels when it hits the tissue, sends this data to a computer, runs it through an algorithm, and produces a straightforward answer as to whether the tissue is cancerous.
“Our big discovery is that we can use the probe’s reading of the fluorescing agent to measure the existence of a low-grade tumor in tissue,” says Dr. Paulsen. “The probe is basically an enabling technology to show that information to the surgeon – a visual aid.”
He says that when they first saw the results of using their fluorescing agent and probe on low-grade brain tumors, it was “jaw-dropping. The tumor glowed like lava.”
The Thayer/Norris Cotton Cancer Center/Dartmouth-Hitchcock Medical Center team, which has been working on the brain probe for about six years in collaboration with researchers from the University of Toronto, built on research that was originally conducted in Germany about 15 years ago. But the German research did not focus on low-grade tumors. The assumption, Dr. Paulsen says, was that, due to the blood-brain barrier, low-grade tumors did not have enough PplX and therefore would not fluoresce.
In a pilot study, Roberts operated on 10 patients with gliomas. He used a microscope throughout the surgery to see the fluorescence and used the hand-held probe to evaluate sections of the tissue where the fluorescence was not definitive. After the surgeries were complete, a pathologist evaluated how accurately the probe had identified tumor tissue.
The results, published in the Journal of Biomedical Optics are striking. Diagnoses based on fluorescence only had an accuracy of 64 percent. But when Roberts used the probe, the accuracy increased to 94 percent, meaning that Roberts was much more successful in differentiating between tumor tissue and normal tissue. Although the study was small, it introduces a promising method to help surgeons remove only what they want and nothing more.
Dr. Paulsen says that a protocol is in place for a similar study on lung cancer tumors. He thinks the brain probe may have applications for other cancers as well, but for now the research will have to proceed one cancer type at a time.
Notes about this brain cancer research article
Support to Dartmouth College and the University of Toronto for this research was provided through National Institutes of Health grants RO1-NS052274-01A2.
Contact: Donna Dubuc – Dartmouth College
Source: Dartmouth-Hitchcock press release
Image Source: Glowing brain tumor image adapted from Dartmouth-Hitchcock press release image
Original Research: Abstract for “Spatial frequency domain tomography of protoporphyrin IX fluorescence in preclinical glioma models” by Soren D. Konecky, Chris M. Owen, Tyler Rice, Pablo A. Valdés, Kolbein Kolste, Brian C. Wilson, Frederic Leblond, David W. Roberts, Keith D. Paulsen and Bruce J. Tromberg in Journal of Biomedical Optics 4 May 2012 doi: 10.1117/1.JBO.17.5.056008







