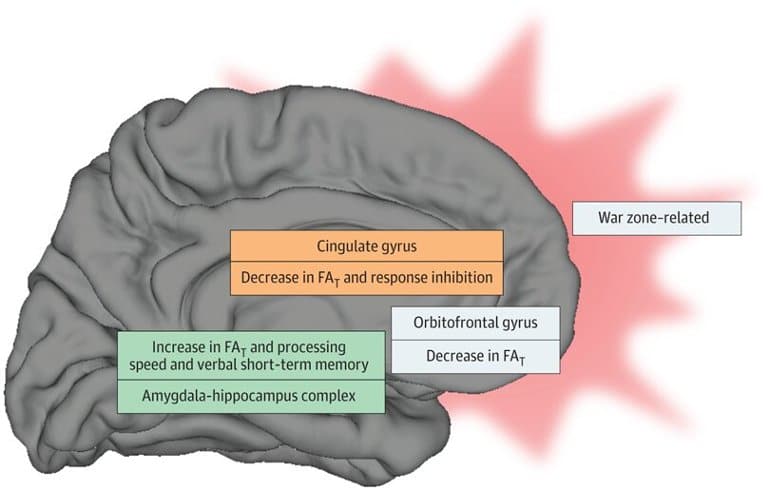
Summary: War zone-related stress was associated with alterations in limbic gray matter microstructure, independent of a mental health or tbi diagnosis. In turn, these alterations were associated with cognitive function, including impaired response inhibition.
Source: Brigham and Women’s Hospital
Military service members who have returned from theaters of war are at increased risk of mental health problems. But few studies have examined the physical effects that war-zone related stress may have on the structure of the brain.
A new study led by investigators at Brigham and Women’s Hospital, a founding member of the Mass General Brigham health care system, investigates microstructural changes in the limbic and paralimbic gray matter regions of the brain—areas that control basic emotions and drives.
The team analyzed diffusion-weighted MRI scans from 168 male veterans who had participated in the Translational Research Center for TBI and Stress Disorders (TRACTS) study, which took place in 2010 to 2014 at the Veterans Affair Rehabilitation Research and Development TBI National Network Research Center.
The team found that war-zone related stress was associated with alterations of the limbic gray matter microstructure, independent of a diagnosis of a mental health disorder or mild traumatic injury. These structural alterations were, in turn, associated with cognitive functioning, including impaired response inhibition as well as improved verbal short-term memory and processing speed.
“These findings suggest that war zone-related stress may lead to microstructure alterations in the brain,” said corresponding author Inga K. Koerte, MD, of the Psychiatry Neuroimaging Laboratory in the Brigham’s Department of Psychiatry.
“These changes may underlie the deleterious outcomes of war zone-related stress on brain health. Given these findings, military service members may benefit from early therapeutic interventions following deployment.”
About this stress and neuroscience research news
Author: Press Office
Source: Brigham and Women’s Hospital
Contact: Press Office – Brigham and Women’s Hospital
Image: The image is in the public domain
Original Research: Open access.
“Association of War Zone–Related Stress With Alterations in Limbic Gray Matter Microstructure” by Elisabeth Kaufmann et al. JAMA Network Open
Abstract
Association of War Zone–Related Stress With Alterations in Limbic Gray Matter Microstructure
Importance
Military service members returning from theaters of war are at increased risk for mental illness, but despite high prevalence and substantial individual and societal burden, the underlying pathomechanisms remain largely unknown. Exposure to high levels of emotional stress in theaters of war and mild traumatic brain injury (mTBI) are presumed factors associated with risk for the development of mental disorders.
Objective
To investigate (1) whether war zone–related stress is associated with microstructural alterations in limbic gray matter (GM) independent of mental disorders common in this population, (2) whether associations between war zone–related stress and limbic GM microstructure are modulated by a history of mTBI, and (3) whether alterations in limbic GM microstructure are associated with neuropsychological functioning.
Design, Setting, and Participants
This cohort study was part of the TRACTS (Translational Research Center for TBI and Stress Disorders) study, which took place in 2010 to 2014 at the Veterans Affair Rehabilitation Research and Development TBI National Network Research Center. Participants included male veterans (aged 18-65 years) with available diffusion tensor imaging data enrolled in the TRACTS study. Data analysis was performed between December 2017 to September 2021.
Exposures
The Deployment Risk and Resilience Inventory (DRRI) was used to measure exposure to war zone–related stress. The Boston Assessment of TBI-Lifetime was used to assess history of mTBI. Stroop Inhibition (Stroop-IN) and Inhibition/Switching (Stroop-IS) Total Error Scaled Scores were used to assess executive or attentional control functions.
Main Outcomes and Measures
Diffusion characteristics (fractional anisotropy of tissue [FAT]) of 16 limbic and paralimbic GM regions and measures of functional outcome.
Results
Among 384 male veterans recruited, 168 (mean [SD] age, 31.4 [7.4] years) were analyzed. Greater war zone–related stress was associated with lower FAT in the cingulate (DRRI-combat left: P = .002, partial r = −0.289; DRRI-combat right: P = .02, partial r = −0.216; DRRI-aftermath left: P = .004, partial r = −0.281; DRRI-aftermath right: P = .02, partial r = −0.219), orbitofrontal (DRRI-combat left medial orbitofrontal cortex: P = .02, partial r = −0.222; DRRI-combat right medial orbitofrontal cortex: P = .005, partial r = −0.256; DRRI-aftermath left medial orbitofrontal cortex: P = .02, partial r = −0.214; DRRI-aftermath right medial orbitofrontal cortex: P = .005, partial r = −0.260; DRRI-aftermath right lateral orbitofrontal cortex: P = .03, partial r = −0.196), and parahippocampal (DRRI-aftermath right: P = .03, partial r = −0.191) gyrus, as well as with higher FAT in the amygdala-hippocampus complex (DRRI-combat: P = .005, partial r = 0.254; DRRI-aftermath: P = .02, partial r = 0.223). Lower FAT in the cingulate-orbitofrontal gyri was associated with impaired response inhibition (Stroop-IS left cingulate: P < .001, partial r = −0.440; Stroop-IS right cingulate: P < .001, partial r = −0.372; Stroop-IS left medial orbitofrontal cortex: P < .001, partial r = −0.304; Stroop-IS right medial orbitofrontal cortex: P < .001, partial r = −0.340; Stroop-IN left cingulate: P < .001, partial r = −0.421; Stroop-IN right cingulate: P < .001, partial r = −0.300; Stroop-IN left medial orbitofrontal cortex: P = .01, partial r = −0.223; Stroop-IN right medial orbitofrontal cortex: P < .001, partial r = −0.343), whereas higher FAT in the mesial temporal regions was associated with improved short-term memory and processing speed (left amygdala-hippocampus complex: P < .001, partial r = −0.574; right amygdala-hippocampus complex: P < .001, partial r = 0.645; short-term memory left amygdala-hippocampus complex: P < .001, partial r = 0.570; short-term memory right amygdala-hippocampus complex: P < .001, partial r = 0.633). A history of mTBI did not modulate the association between war zone–related stress and GM diffusion.
Conclusions and Relevance
This study revealed an association between war zone–related stress and alteration of limbic GM microstructure, which was associated with cognitive functioning. These results suggest that altered limbic GM microstructure may underlie the deleterious outcomes of war zone–related stress on brain health. Military service members may benefit from early therapeutic interventions after deployment to a war zone.







