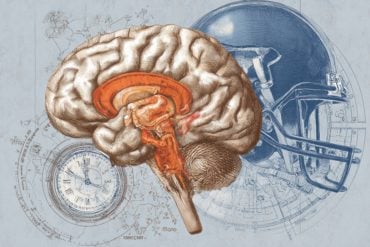
Summary: After eating contaminated food, toxins activate the release of serotonin by the enterochromaffin cells on the lining of the intestinal lumen. The serotonin binds to receptors on vagal sensory neurons in the gut, transmitting signals along the vagus nerve to neurons in the dorsal vagal complex, inducing retching behaviors.
Source: Cell Press
The urge to vomit after eating contaminated food is the body’s natural defensive response to get rid of bacterial toxins. However, the process of how our brain initiates this biological reaction upon detecting the germs remains elusive.
For the first time, researchers mapped out the detailed neural pathway of the defensive responses from the gut to the brain in mice.
The study, presented November 1 in the journal Cell, could help scientists develop better anti-nausea medications for cancer patients who undergo chemotherapy.
Many foodborne bacteria produce toxins in the host after being ingested. The brain, after sensing their presence, will initiate a series of biological responses, including vomit and nausea, to get rid of the substances and develop an aversion toward foods that taste or look the same.
“But details on how the signals are transmitted from the gut to the brain were unclear, because scientists couldn’t study the process on mice,” says Peng Cao, the paper’s corresponding author at the National Institute of Biological Sciences in Beijing. Rodents cannot vomit, likely because of their long esophagus and weaker muscle strength compared to their body size.
As a result, scientists have been studying vomit in other animals like dogs and cats, but these animals are not comprehensively studied and thus failed to reveal the mechanism of nausea and vomiting.
Cao and his team noticed that while mice don’t vomit, they retch—meaning they also experience the urge to vomit without throwing up.
The team found that after receiving Staphylococcal enterotoxin A (SEA), which is a common bacterial toxin produced by Staphylococcus aureus that also leads to foodborne illnesses in humans, mice developed episodes of unusual mouth opening.
Mice that received SEA opened their mouths at angles wider than those observed in the control group, where mice received saline water. Moreover, during these episodes, the diaphragm and abdominal muscles of the SEA-treated mice contract simultaneously, a pattern seen in dogs when they are vomiting. During normal breathing, animals’ diaphragm and abdominal muscles contract alternatively.
“The neural mechanism of retching is similar to that of vomiting. In this experiment, we successfully build a paradigm for studying toxin-induced retching in mice, with which we can look into the defensive responses from the brain to toxins at the molecular and cellular levels,” Cao says.
In mice treated with SEA, the team found the toxin in the intestine activates the release of serotonin, a type of neurotransmitter, by the enterochromaffin cells on the lining of the intestinal lumen.
The released serotonin binds to the receptors on the vagal sensory neurons located in the intestine, which transmits the signals along the vagus nerves from the gut to a specific type of neurons in the dorsal vagal complex—Tac1+DVC neurons—in the brainstem.
When Cao and his team inactivated the Tac1+DVC neurons, SEA-treated mice retched less compared with mice with normal Tac1+DVC neuron activities.
In addition, the team investigated whether chemotherapy drugs, which also induce defensive responses like nausea and vomiting in recipients, activate the same neural pathway.

They injected mice with doxorubicin, a common chemotherapy drug. The drug made mice retch, but when the team inactivated their Tac1+ DVC neurons or serotonin synthesis of their enterochromaffin cells, the animals’ retching behaviors were significantly reduced.
Cao says some of the current anti-nausea medications for chemotherapy recipients, such as Granisetron, work by blocking the serotonin receptors. The study helps explain why the drug works.
“With this study, we can now better understand the molecular and cellular mechanisms of nausea and vomiting, which will help us develop better medications,” Cao says.
Next, Cao and his colleagues want to explore how toxins act on enterochromaffin cells. Preliminary research shows that enterochromaffin cells don’t sense the presence of toxins directly. The process likely involves complex immune responses of damaged cells in the intestine.
“In addition to foodborne germs, humans encounter a lot of pathogens, and our body is equipped with similar mechanisms to expel these toxic substances.
“For example, coughing is our body’s attempt to remove the coronavirus. It’s a new and exciting field of research about how the brain senses the existence of pathogens and initiates responses to get rid of them,” Cao says, adding that future research may reveal new and better targets for drugs, including anti-nausea medicines.
About this neuroscience research news
Author: Press Office
Source: Cell Press
Contact: Press Office – Cell Press
Image: The image is in the public domain
Original Research: Open access.
“The gut-to-brain axis for toxin-induced defensive responses” by Peng Cao et al. Cell
Abstract
The gut-to-brain axis for toxin-induced defensive responses
Highlights
- Mice exhibit nausea and retching to bacterial toxins and chemotherapeutic drugs
- Identification of a molecularly defined gut-to-brain circuit for nausea and retching
- Distinct brainstem circuits drive nausea and retching
- Toxin-induced signals may be mediated via an immune-neuroendocrine axis in the gut
Summary
After ingestion of toxin-contaminated food, the brain initiates a series of defensive responses (e.g., nausea, retching, and vomiting). How the brain detects ingested toxin and coordinates diverse defensive responses remains poorly understood.
Here, we developed a mouse-based paradigm to study defensive responses induced by bacterial toxins. Using this paradigm, we identified a set of molecularly defined gut-to-brain and brain circuits that jointly mediate toxin-induced defensive responses.
The gut-to-brain circuit consists of a subset of Htr3a+ vagal sensory neurons that transmit toxin-related signals from intestinal enterochromaffin cells to Tac1+ neurons in the dorsal vagal complex (DVC).
Tac1+ DVC neurons drive retching-like behavior and conditioned flavor avoidance via divergent projections to the rostral ventral respiratory group and lateral parabrachial nucleus, respectively. Manipulating these circuits also interferes with defensive responses induced by the chemotherapeutic drug doxorubicin.
These results suggest that food poisoning and chemotherapy recruit similar circuit modules to initiate defensive responses.