Summary: A large-scale Canadian study has found that older adults who sustain traumatic brain injuries (TBI) face a significantly higher risk of developing dementia, needing home care, or being admitted to long-term care. Researchers found that TBIs, most commonly caused by falls, increase dementia risk by up to 69% in the first five years following injury.
The study also revealed disparities based on sex, age, and income, with women and individuals from low-income areas particularly vulnerable. These findings underscore the need for fall prevention programs and targeted community-based dementia support for at-risk seniors.
Key Facts:
- Elevated Dementia Risk: Older adults with a TBI were 69% more likely to develop dementia within five years compared to those without.
- Gender and Income Disparities: Women, older adults (especially 85+), and those from low-income regions faced higher dementia risks and greater care needs.
- Preventable Cause: Over half of TBIs in seniors result from falls, highlighting opportunities for prevention and early intervention.
Source: CAMJ
Traumatic brain injuries (TBI) in older adults are associated with new cases of dementia, use of home care services, and admission to long-term care, according to new research published in CMAJ (Canadian Medical Association Journal).
“One of the most common reasons for TBI in older adulthood is sustaining a fall, which is often preventable,” write Dr. Yu Qing Huang, ICES PhD student, and Dr. Jennifer Watt, associate professor and ICES scientist, both geriatricians at St. Michael’s Hospital, Unity Health, and affiliated with the University of Toronto, along with their coauthors.
“By targeting fall-related TBIs, we can potentially reduce TBI-associated dementia in this population.”
Traumatic brain injuries are caused by a direct impact to the head or indirect force (e.g., whiplash) with one of the following: loss of consciousness, posttraumatic amnesia, disorientation, or neurological signs like slurred speech, muscle weakness, or vision changes. More than 50% of TBIs in older adults result from falls, and 1 million people in Canada over age 65 will experience a TBI in their lifetime.
To understand the impact of late-life TBI and the association with new cases of dementia and related care needs, researchers analyzed data on more than 260 000 adults aged 65 years or older with and without TBI between April 2004 and March 2020. The study followed participants until a diagnosis of dementia, to March 2021, or death.
New TBI was associated with a 69% increased risk of subsequent dementia in the first 5 years, a 56% increased risk beyond 5 years, and more days of publicly funded home care (87 days compared with 84 days in people without TBI).
Age and female sex were associated with higher risk of dementia, with about 1 in 3 people aged 85 years and older predicted to develop dementia after TBI. Income was also linked to dementia risk, with people from low-income neighbourhoods at higher risk of dementia than those in high-income neighbourhoods.
People living in smaller communities, low-income regions, and areas with less ethnic diversity were more likely to be admitted to a long-term care facility.
“Our findings suggest that, to better align limited health resources with population needs, specialized programs such as community-based dementia prevention programs, and support services should be prioritized for female older adults (≥ 75) living in smaller communities and low-income and low-diversity areas.”
The authors intend for these results to help clinicians and families navigate the effects of a TBI.
“Although TBI has been studied as a risk factor for dementia in adulthood, our findings emphasize its significant association with an increased rate of incident dementia, even when it is sustained in late life, and how this risk changes over time,” write the authors.
“This critical information can assist clinicians in guiding older patients and their families to better understand long-term risks.”
Key Questions Answered:
A: Most TBIs in seniors are caused by falls, many of which are preventable through safety measures and balance-focused interventions.
A: A TBI increases dementia risk by up to 69% in the first five years after injury and 56% beyond that period, even when sustained later in life.
A: Women, adults over 75, and individuals from smaller, low-income, or less diverse communities face the greatest risks of dementia and long-term care admission after TBI.
About this TBI and dementia research news
Author: Kim Barnhardt
Source: CAMJ
Contact: Kim Barnhardt – CAMJ
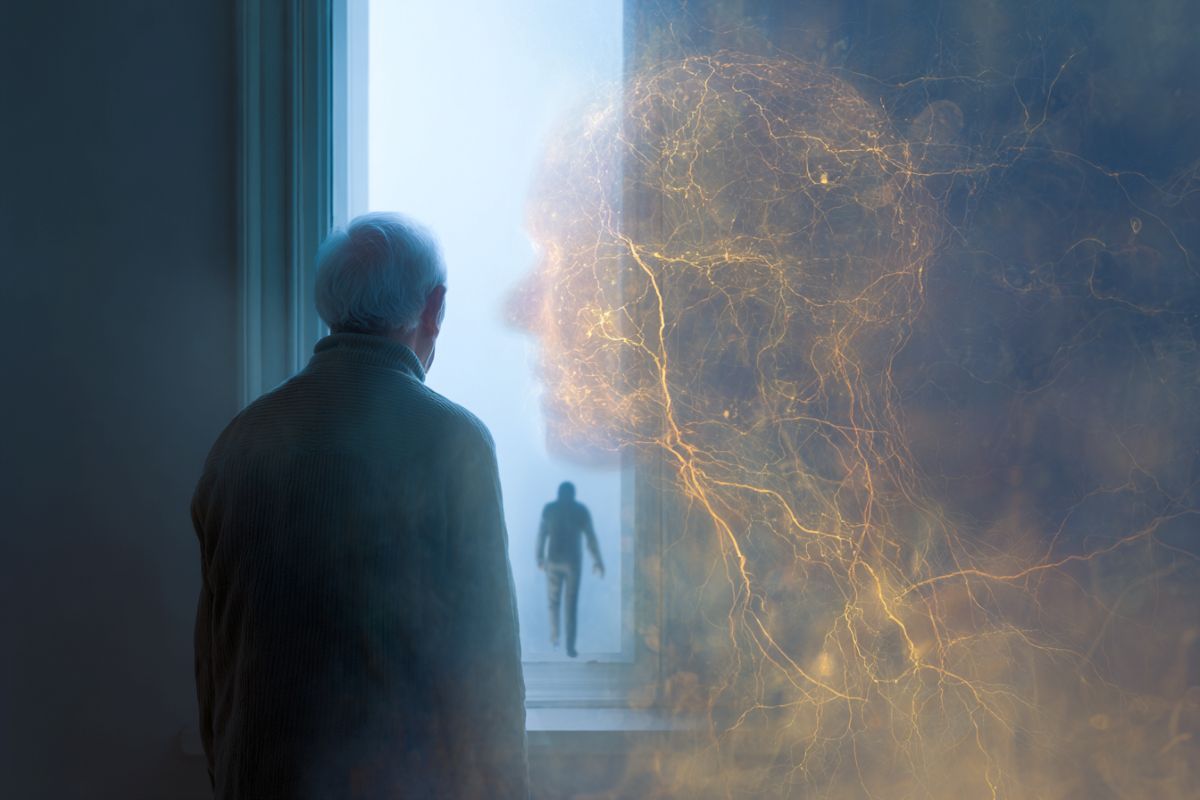
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Rate of incident dementia and care needs among older adults with new traumatic brain injury: a population-based cohort study” by Yu Qing Huang et al. CAMJ
Abstract
Rate of incident dementia and care needs among older adults with new traumatic brain injury: a population-based cohort study
Background: The long-term impacts of traumatic brain injury (TBI) in older adults are not well known. Our objective was to describe the association between late-life TBI, incident dementia, and health care needs.
Methods: We conducted a retrospective cohort study using linked health administrative data in Ontario, Canada, and included community-dwelling individuals older than 65 years with a new TBI between Apr. 1, 2004, and Mar. 1, 2020, and up to 17 years of follow-up. People with and without TBI were 1:1 matched on age, sex, and propensity score.
We compared rates of incident dementia (≤ 5 yr and > 5 yr), use of publicly funded home care, and admission to a long-term care home, using cause-specific hazard models. We used conditional inference trees to identify subgroups at high risk for outcomes based on associations with individual and intersecting social determinants of health.
Results: We included 132 113 matched pairs. Late-life TBI was associated with an increased rate of incident dementia (≤ 5 yr: hazard ratio [HR] 1.69, 95% confidence interval [CI] 1.66 to 1.72; > 5 yr: HR 1.56, 95% CI 1.53 to 1.59), use of publicly funded home care (HR 1.30, 95% CI 1.29 to 1.31), and admission to a long-term care home (HR 1.45, 95% CI 1.42 to 1.47).
Dementia was more common among older females from low-income neighbourhoods than among male peers (29.0% v. 24.7%). Residents of smaller communities received less home care than those in larger communities (60.1% v. 64.6%) and had a higher probability of long-term care home admission (26.3% v. 21.7%).
Interpretation: Late-life TBI in community-dwelling older adults is associated with higher rates of incident dementia, use of publicly funded home care, and admission to a long-term care home, with older females and residents of smaller communities experiencing poorer outcomes. Clinical awareness and policy planning that reflects these needs and population heterogeneity are important.
Protocol registration: Open Science Framework identifier 10.17605/OSF.IO/KZT3F






