Summary: An opinion article reports on a potential common cause for both SIDS and SUDEP. The reason sudden death may occur is due to a person’s inability to wake when CO2 levels in the blood rise, as a result of dysfunctional serotonin neurons in the midbrain.
Source: Cell Press
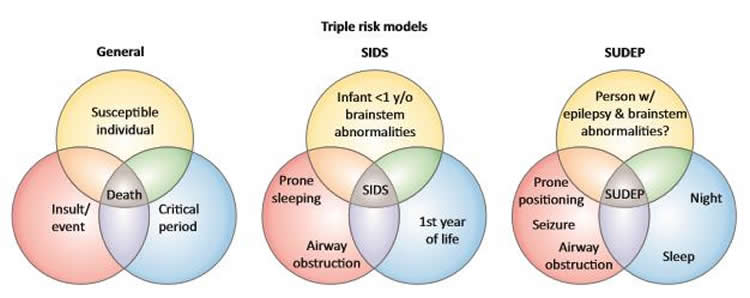
Sudden Infant Death Syndrome (SIDS) and Sudden Unexpected Death in Epilepsy (SUDEP) are syndromes that share many medical similarities but whose physiological causes are poorly understood. An opinion article publishing March 21 in the journal Trends in Neuroscience suggests that the inability for an individual to wake up when their CO2 blood levels rise, likely due to a faulty neural reflex, maybe a shared cause for incidences of death in both disorders.
“If someone’s airway is blocked with a blanket, for example, they are unable to expel CO2, which causes their CO2 blood levels to rise. Normally, this triggers a series of reactions that cause the individual to wake up and either re-position themselves so that they can breathe again, or cry out for help, like in the case of a baby,” says author Gordon Buchanan, an associate professor of neurology at the University of Iowa. “However, in instances of SIDS and SUDEP, evidence is beginning to suggest that elevated CO2 doesn’t trigger this wake-up response like it should, which can ultimately result in death.”
Why a person would fail to wake up from increased CO2 is not fully understood, but a potential explanation is that a malfunctioning serotonin receptor in the midbrain may be responsible.
“Serotonin neurons in the medulla are involved in regulation of breathing, and we think the ones in the midbrain are involved in regulating a person’s ability to wake up,” says Buchanan. “In instances of SIDS and SUDEP, autopsies frequently reveal that there are abnormalities in the individual’s serotonin system in the brain.
“It is very possible that there is a direct path by which CO2 is sensed by serotonin receptors in the midbrain, and when there is too much CO2 present, the brain reacts by waking up the individual,” he says. “The existence of this direct pathway is important because it could drive future treatments.”
However, applying this information to create preventative therapies for these syndromes is still in the works. In addition to validating that SIDS and SUDEP are caused by an inability to wake up because of a defective CO2 system, a safe and reliable way to test if a person has dysfunctional serotonin receptors needs to be developed as well. Currently, such determinations are possible only through autopsies.
In the meantime, parents or caregivers for infants or people with epilepsy should employ the same preventative measures that have been recommended, and largely successful, for decades. “For infants six months and younger, which is the population most susceptible to SIDS, parents should put babies on their backs to sleep. At that age, they can’t really roll, so they should stay put through the night,” Buchanan says. Further, not putting plush toys or blankets in the crib and dressing the baby in tight-fitting clothing are other guidelines to follow.
“As for people with epilepsy who may be prone to SUDEP, which tends to be people who have nighttime seizures, they can also try to sleep on their backs, although it’s less likely that they’ll stay like that throughout the night since they can roll,” says Buchanan. “And in both cases, using a baby monitor to keep an eye on the individual can be helpful.”
Funding: Buchanan is supported by the NIH/NINDS; the Pappajohn Biomedical Institute and Iowa Neuroscience Institute at the University of Iowa; and the Beth Levitt Tross Professorship in Epilepsy Research.
Source:
Cell Press
Media Contacts:
Brianne Fagan – Cell Press
Image Source:
The image is credited to Buchanan et al.Trends in Neurosciences.
Original Research: The study will appear in Trends in Neurosciences.







