Summary: Spinal cord injuries have long been considered permanent because neurons in the central nervous system lack the natural ability to regrow. However, researchershave developed a novel, 3D-printed implant that could change that.
The study details a multifunctional scaffold designed to mimic the spinal cord’s physical structure while delivering tiny RNA-loaded particles. These particles “silence” a specific gene called PTEN, which acts as a biological brake on nerve regrowth. By removing this internal barrier and providing physical support, the implant significantly enhanced neuron growth in laboratory models, offering a new path toward restoring function after paralysis.
Key Facts
- The Dual-Action Scaffold: The implant provides both a physical 3D structure for cells to latch onto and a biological signal to trigger repair.
- Silencing the Brake: The implant delivers siRNA to silence the PTEN gene, which is responsible for suppressing the regenerative capacity of neurons after an injury.
- Biomimetic Design: The 3D-printed structure is engineered to match the specific stiffness and anatomy of the human spinal cord to prevent further tissue damage and encourage integration.
- Nerve Regrowth: In lab models, injured neurons exposed to the RNA-activated implant showed a “significantly enhanced” capacity to grow across the injury site.
- Patient-Centered Research: The project was developed with input from the Irish Rugby Football Union Charitable Trust, ensuring the research remains relevant to the needs of those living with spinal cord injuries.
Source: RCSI
Researchers from RCSI University of Medicine and Health Sciences have developed a novel implant that delivers tiny growth-promoting particles directly to injured nerve cells, helping them to regrow after spinal cord injury.
The study, published in the journal Bioactive Materials, shows how a 3D implant designed to mimic the structure and stiffness of the spinal cord can be combined with tiny particles engineered to carry RNA to encourage nerve cells (neurons) to grow.
The work was led by researchers at RCSI’s Tissue Engineering Research Group (TERG) and the Research Ireland Centre for Advanced Materials and BioEngineering Research (AMBER).
Spinal cord injuries often result in permanent paralysis because damaged neurons in the central nervous system have a very limited capacity to regrow. While biomaterial implants can provide physical support at the injury site, these cells also face molecular barriers that prevent their regrowth.
To overcome this, the team developed a multifunctional implant that not only supports regenerating tissue but also delivers RNA-based signals that encourage neurons to switch their growth mechanisms back on.
These signals target one such barrier, a gene called PTEN, which is known to suppress neuron regrowth after injury. By silencing PTEN at the injury site, the implant helps remove an internal barrier to repair in these cells.
“We’ve created an environment that both physically and biologically re-enhances the regenerative capacity of injured neurons, which is a key requirement for restoring function after spinal cord injury,” said Professor Fergal O’Brien, Deputy Vice Chancellor for Research and Innovation, Professor of Bioengineering and Regenerative Medicine and Head of RCSI TERG.
“In laboratory models of spinal cord injury, neurons exposed to the RNA-activated implant showed significantly enhanced growth.”
The research was developed with guidance from an advisory panel supported by the Irish Rugby Football Union Charitable Trust (IRFU-CT), bringing together people living with spinal cord injury, clinicians, neuroscientists and engineers to shape research priorities and ensure relevance to patients’ real-world needs.
“While this study focused on laboratory models, the next steps will to be to test the approach in vivo and explore how RNA-activated biomaterials could help bridge damaged spinal cord tissue and restore lost connections,” said Dr Tara McGuire who carried out the research as a PhD student in TERG.
Funding: The study was supported by the IRFU-CT and Research Ireland with additional funding from the Anatomical Society and the Health Research Board.
Key Questions Answered:
A: Unlike the rest of your body, the central nervous system has “internal brakes”—like the PTEN gene—that actively stop neurons from growing once you reach adulthood. This evolved to keep the brain’s wiring stable, but it makes injury recovery nearly impossible without intervention.
A: Think of it like a molecular “mute” button. The siRNA delivered by the implant tells the cell to stop producing the PTEN protein. Without that protein to hold them back, the neurons “switch on” their growth mechanisms and start reaching out to reconnect.
A: Not yet. The research has shown incredible success in laboratory models. The next phase involves in vivo testing to see if the “RNA bridge” can successfully restore movement and sensation in living subjects.
Editorial Notes:
- This article was edited by a Neuroscience News editor.
- Journal paper reviewed in full.
- Additional context added by our staff.
About this spinal cord injury and neurotech research news
Author: Laura Anderson
Source: RCSI
Contact: Laura Anderson – RCSI
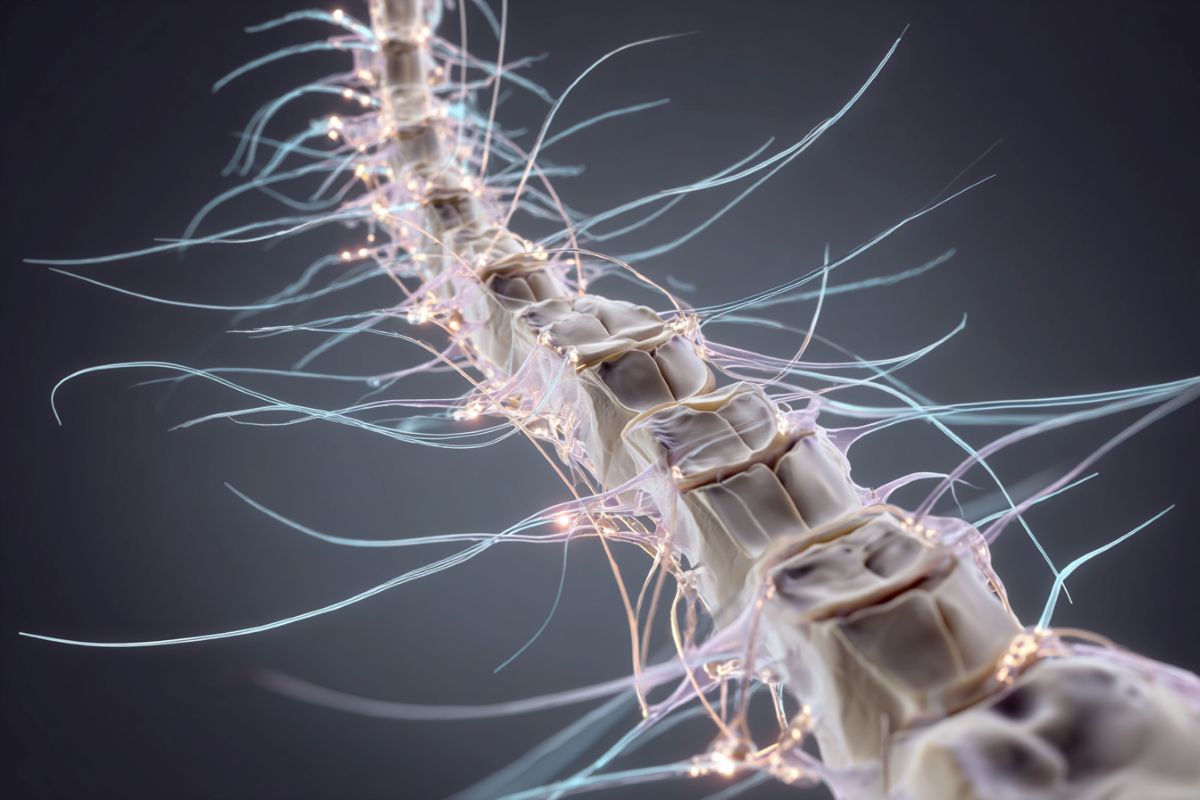
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Development of a PTEN-siRNA activated scaffold to promote axonal regrowth following spinal cord injury” by Tara K. McGuire, Martyna Stasiewicz, Cian O’Connor, Ian Woods, Jack Maughan, Marko Dobricic, Giulio Brunetti, James E. Dixon, Adrian G. Dervan, and Fergal J. O’Brien. Bioactive Materials
DOI:10.1016/j.bioactmat.2026.01.022
Abstract
Development of a PTEN-siRNA activated scaffold to promote axonal regrowth following spinal cord injury
This study showcases the successful development of a PTEN-siRNA activated scaffold for SCI repair applications.
Initially, siRNA was combined with the novel non-viral glycosaminoglycan-binding enhanced transduction (GET) peptide vector (image of GET vector from [22]).
The formulated GET-siRNA nanoparticles effectively transfected primary neurons, a cell type generally considered challenging to transfect.
Subsequently, siRNA-nanoparticles were incorporated into a hyaluronic acid scaffold enriched with neurotrophic extracellular matrix proteins (collagen IV and fibronectin) developed by our laboratory for spinal cord repair applications.
Functionalisation of these scaffolds with PTEN-siRNA nanoparticles significantly enhanced their capacity to promote neurite outgrowth.






