Summary: Researchers discover 8 genes that could explain the inverse relationship between RA and schizophrenia.
Source: University of Pittsburgh.
An in-depth computational analysis of genetic variants implicated in both schizophrenia and rheumatoid arthritis by researchers at the University of Pittsburgh points to eight genes that may explain why susceptibility to one of the disorders could place individuals at lower risk for the other, according to the results of a study published today in the journal npj Schizophrenia.
“There is a wealth of genomic data on both schizophrenia and rheumatoid arthritis. Analyzing it jointly with known protein interaction information could provide invaluable clues to the relationship between the diseases and also shed light on their shared roots,” said Madhavi Ganapathiraju Ph.D., associate professor of biomedical informatics at the University of Pittsburgh School of Medicine and senior author of the study.
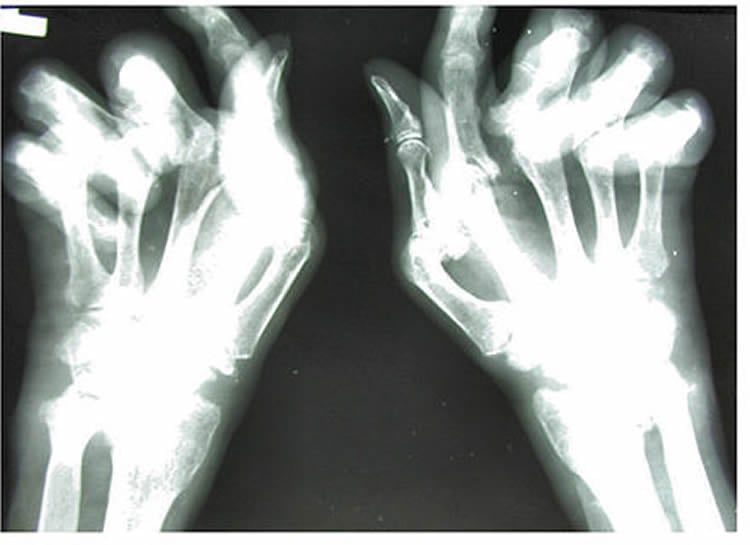
While schizophrenia is a psychiatric disorder of unknown origin and rheumatoid arthritis is an autoimmune disease of the joints that occurs as a result of the body’s immune system attacking its own cells, both disorders are thought to be influenced by multiple genetic risk factors modified by the environment.
“Several previous research studies have hinted at a potential inverse relationship in the prevalence and risk for the two disorders, so we wondered if individual genetic variants may exist that could have opposing effects on the risk of schizophrenia and rheumatoid arthritis,” said co-senior author Vishwajit Nimgaonkar M.D., Ph.D., professor of psychiatry at Pitt’s School of Medicine and human genetics at Pitt’s Graduate School of Public Health.
The researchers first analyzed two large databases of genetic variants significantly associated with either schizophrenia or rheumatoid arthritis. They identified 18 unique variants, also known as single nucleotide polymorphisms (SNPs) that were located in the HLA region of the genome that harbors genes associated with immune function. The variants appeared to confer different risk for schizophrenia or rheumatoid arthritis. As the SNPs were located near eight known genes in this region, the authors suggested those genes might lead to dysfunction in both schizophrenia and rheumatoid arthritis. Proteins encoded by two of these eight genes, HLA-B and HLA-C, are present in both brain and immune cells.
Analysis of proteins that interact with these eight genes using a computational model developed last year by Ganapathiraju’s team called High-Precision Protein Interaction Prediction found more than 25 signaling pathways with proteins common to both rheumatoid arthritis and schizophrenia signaling. Moreover, several of these pathways were associated with immune system function and inflammation.
The findings are encouraging because they support associations of the HLA gene region and immune function with schizophrenia and rheumatoid arthritis that were known over four decades ago, said Ganapathiraju. Increasing evidence also suggests that a dysfunctional immune system could play a role in the development of schizophrenia.
“We believe that the research community studying these two disorders will find our results extremely helpful,” Nimgaonkar said.
The authors note that the study only focused on SNPs in known gene regions, and other mechanisms apart from the ones they described may also contribute to the diseases. However, the study has significantly narrowed the list of potential genes for examining the schizophrenia/rheumatoid arthritis relationship. Studying the functional relevance of the gene candidates in cells and tissues will provide insights into the two disorders, according to the researchers.
Other study authors included Tulsi A. Malavia, Srilakshmi Chaparala, Joel Wood, Kodavalli Chowdari, Ph.D., Konasale M. Prasad, M.D., and Lora McClain, Ph.D., all of Pitt; and Anil G. Jegga, D.V.M., of Cincinnati Children’s Hospital.
Funding: The research was funded by National Institutes of Health grants MH93480, MH093246, MH084053 and MH094564.
Source: Arvind Suresh – University of Pittsburgh
Image Source: NeuroscienceNews.com image is credited to OpenStax College and is licensed CC by 3.0.
Original Research: Full open access research “Generating testable hypotheses for schizophrenia and rheumatoid arthritis pathogenesis by integrating epidemiological, genomic, and protein interaction data” by Tulsi A. Malavia, Srilakshmi Chaparala, Joel Wood, Kodavali Chowdari, Konasale M. Prasad, Lora McClain, Anil G. Jegga, Madhavi K. Ganapathiraju & Vishwajit L. Nimgaonkar in NPJ: Schizophrenia. Published online February 24 2017 doi:10.1038/s41537-017-0010-z
[cbtabs][cbtab title=”MLA”]University of Pittsburgh “Clues to Relationship Between Schizophrenia and Rheumatoid Arthritis.” NeuroscienceNews. NeuroscienceNews, 25 February 2017.
<https://neurosciencenews.com/schizophrenia-ra-6158/>.[/cbtab][cbtab title=”APA”]University of Pittsburgh (2017, February 25). Clues to Relationship Between Schizophrenia and Rheumatoid Arthritis. NeuroscienceNew. Retrieved February 25, 2017 from https://neurosciencenews.com/schizophrenia-ra-6158/[/cbtab][cbtab title=”Chicago”]University of Pittsburgh “Clues to Relationship Between Schizophrenia and Rheumatoid Arthritis.” https://neurosciencenews.com/schizophrenia-ra-6158/ (accessed February 25, 2017).[/cbtab][/cbtabs]
Abstract
Generating testable hypotheses for schizophrenia and rheumatoid arthritis pathogenesis by integrating epidemiological, genomic, and protein interaction data
Patients with schizophrenia and their relatives have reduced prevalence of rheumatoid arthritis. Schizophrenia and rheumatoid arthritis genome-wide association studies also indicate negative genetic correlations, suggesting that there may be shared pathogenesis at the DNA level or downstream. A portion of the inverse prevalence could be attributed to pleiotropy, i.e., variants of a single nucleotide polymorphism that could confer differential risk for these disorders. To study the basis for such an interrelationship, we initially compared lists of single nucleotide polymorphisms with significant genetic associations (p < 1e-8) for schizophrenia or rheumatoid arthritis, evaluating patterns of linkage disequilibrium and apparent pleiotropic risk profiles. Single nucleotide polymorphisms that conferred risk for both schizophrenia and rheumatoid arthritis were localized solely to the extended HLA region. Among single nucleotide polymorphisms that conferred differential risk for schizophrenia and rheumatoid arthritis, the majority were localized to HLA-B, TNXB, NOTCH4, HLA-C, HCP5, MICB, PSORS1C1, and C6orf10; published functional data indicate that HLA-B and HLA-C have the most plausible pathogenic roles in both disorders. Interactomes of these eight genes were constructed from protein–protein interaction information using publicly available databases and novel computational predictions. The genes harboring apparently pleiotropic single nucleotide polymorphisms are closely connected to rheumatoid arthritis and schizophrenia associated genes through common interacting partners. A separate and independent analysis of the interactomes of rheumatoid arthritis and schizophrenia genes showed a significant overlap between the two interactomes and that they share several common pathways, motivating functional studies suggesting a relationship in the pathogenesis of schizophrenia/rheumatoid arthritis.
“Generating testable hypotheses for schizophrenia and rheumatoid arthritis pathogenesis by integrating epidemiological, genomic, and protein interaction data” by Tulsi A. Malavia, Srilakshmi Chaparala, Joel Wood, Kodavali Chowdari, Konasale M. Prasad, Lora McClain, Anil G. Jegga, Madhavi K. Ganapathiraju & Vishwajit L. Nimgaonkar in NPJ: Schizophrenia. Published online February 24 2017 doi:10.1038/s41537-017-0010-z







