Summary: Why do some people with a genetic risk for Parkinson’s disease remain healthy while others develop debilitating symptoms? Researchers at discovered that it takes two “partners in crime” to drive neurodegeneration.
In a study using fruit flies, the team found that while a mutation in the common Parkinson’s risk gene GBA1 alone isn’t enough to cause disease, pairing it with a second mutation in the ATP13A2 gene (known as anne in flies) triggers a progressive loss of neurons. The study reveals a toxic “garbage overflow” system: neurons with failing lysosomes produce excess fat molecules that overwhelm the brain’s protective glial cells, leading to inflammation and eventual neural death.
Key Facts
- The Two-Hit Hypothesis: One mutant copy of GBA1 increases risk, but a second factor—a mutation in ATP13A2—is required to actually trigger the disease.
- Cellular Sabotage: GBA1 works mainly in glial cells (the brain’s support system), while ATP13A2 works in neurons.
- Glucosylceramide Buildup: In the dual-mutation model, neurons produce an excess of the fat molecule GlcCer, which is transferred to glial cells until they become overwhelmed and swell.
- Recycling Failure: The research focuses on lysosomes, the cell’s recycling centers. When these fail in both neurons and glia, the brain’s waste-management system collapses.
- Potential Pathways: Treatment with drugs that improve lysosome function or reduce fat production successfully lowered the toxic buildup in lab models, offering new targets for future human therapies.
Source: Baylor College of Medicine
Parkinson’s disease (PD) is the second most common neurodegenerative disease after Alzheimer’s disease, affecting more than 10 million people worldwide. People with this condition may experience tremors, limb stiffness, gait and balance problems and move slowly, like when buttoning a shirt or walking. These symptoms happen because certain brain cells die over time.
Although scientists have known some of the factors that raise a person’s risk, the question remains of why some people with genetic risk factors develop the disease while others never do.

A team at Baylor College of Medicine, the Duncan Neurological Research Institute (Duncan NRI) at Texas Children’s Hospital and collaborating institutions found in the laboratory fruit fly that it takes two mutant genes to drive neurodegeneration. People and fruit flies have two copies of each gene in most cells. Flies without one copy of the Gba1b gene, a common and potent PD genetic risk factor, do not develop neurological problems.
However, neurodegeneration occurs when flies lack both a copy of Gba1b and one copy of anne (the fruit fly equivalent of the human gene ATP13A2). Importantly, the researchers identified multiple PD individuals carrying ATP13A2 and GBA1 variants.
The study appeared in Molecular Neurodegeneration.
“We knew from human studies that people carrying one copy of mutant GBA1 and one copy of normal GBA1 gene have a 5-fold increase in the risk of developing PD, but do not always develop the condition,” said corresponding author Dr. Hugo Bellen, Distinguished Service Professor of molecular and human genetics at Baylor and chair in neurogenetics in the Duncan NRI. “A second factor must be in place for the condition to arise.”
The researchers looked for the second factor among genes linked to lysosomes, structures inside cells responsible for breaking down and recycling cellular material, because many PD risk genes like GBA1 also are linked to lysosomes.
“We found that carrying one mutant copy of Gba1b and one mutant copy of anne drives a slow, progressive neurodegeneration in flies. The flies developed movement problems, lost neurons and showed disruption in the communication between neurons and glia,” said first author Dr. Mingxue Gu, a postdoctoral associate in the Bellen lab.
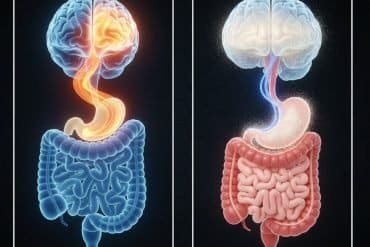
A closer look at the process leading to neurodegeneration revealed that Gba1b and anne work on different cell types. Gba1b works mainly in glial cells, which support and protect neurons, and anne works mostly in neurons, which send electric signals that sustain neural networks. But how can problems in two different cell types lead to neurodegeneration?
Short staffed and overwhelmed
“One surprising result was that the earliest signs of damage didn’t appear in neurons but in glial cells,” Gu said. “These cells began swelling, detaching from nearby neurons, and showing signs of distress. We tied this to accumulation of a fat molecule called glucosylceramide (GlcCer) in glial lysosomes.”
In flies also carrying a mutant anne, lysosomes in the neurons failed to maintain proper acidity. This caused neurons to produce excess GlcCer, which was then transferred to glial cells in amounts far beyond what glia can handle.
As a result, waste materials piled up in glial cells, leading to swelling and structural damage. Without healthy glia to support and protect them, neurons eventually failed, especially those involved in vision and movement. The flies developed movement problems, lost neurons, and showed signs similar to early Parkinson’s disease.
Potential solutions
“One important finding was that we found ways to help reduce the damage,” Bellen said.
Treatment with ML SA1, a drug that improves lysosome function, restored lysosomes’ healthier activity, and myriocin, which reduces GlcCer production, lowered toxic buildup.
Other contributors to this work include Jinghan Zhao, Mingxi Deng, Guang Lin, Xueyang Pan, Wenwen Lin, Mengqi Ma, Jinyong Kim, Seul Kee Byeon, Akhilesh Pandey, Lara M. Lange, Chad A. Shaw, Jonggeol Kim, Joanne Trinh, Christine Klein, Oguz Kanca and Joshua M. Shulman. The authors are affiliated with one or more of the following institutions: Baylor College of Medicine, Duncan NRI, Mayo Clinic, Anipal Academy of Higher Education – India, University of Luebeck – Germany and National Institute of Aging.
Funding: This study was supported by the Huffington Foundation, the Duncan NRI, NIH grants U01CA271410 and 1468 P30CA15083, and DBT/ Wellcome Trust India Alliance (grant IA/CRC/20/1/600002). Further support was provided by the Intramural Research Program of the National Institute on Aging, National Institutes of Health, Department of Health and Human Services (grants ZO1 AG000535 and ZIA AG000949), the Silverstein Foundation for PD with GBA1 and a National Institute of Child Health & Human Development grant (U54 HD083092).
Key Questions Answered:
A: No. This study explains why many carriers stay healthy. It suggests that your brain can handle one “broken” gene, but when a second specific gene also malfunctions, the cumulative stress becomes too much for your brain’s waste-management system to handle.
A: Every cell has lysosomes that act like garbage disposals. In Parkinson’s, these disposals break down. This study shows that when neurons start dumping their “trash” (fat molecules) onto nearby support cells (glia) that are already struggling, the whole neighborhood—the neural network—eventually fails.
A: While not an immediate cure, the researchers successfully used drugs to help the “recycling centers” work better and to stop the excess “trash” from being made. This opens up a clear biological roadmap for developing new Parkinson’s treatments.
Editorial Notes:
- This article was edited by a Neuroscience News editor.
- Journal paper reviewed in full.
- Additional context added by our staff.
About this genetics and Parkinson’s disease research news
Author: Ana María Rodríguez, Ph.D.
Source: Baylor College of Medicine
Contact: Ana María Rodríguez, Ph.D. – Baylor College of Medicine
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Two lysosomal genes ATP13A2 and GBA1 interact to drive neurodegeneration” by Mingxue Gu, Jinghan Zhao, Mingxi Deng, Guang Lin, Xueyang Pan, Wenwen Lin, Mengqi Ma, Jinyong Kim, Seul Kee Byeon, Akhilesh Pandey, Lara M. Lange, Chad A. Shaw, Jonggeol Kim, Joanne Trinh, Christine Klein, Oguz Kanca, Joshua M. Shulman & Hugo J. Bellen. Molecular Neurodegeneration
DOI:10.1186/s13024-025-00923-z
Abstract
Two lysosomal genes ATP13A2 and GBA1 interact to drive neurodegeneration
Background
Parkinson’s disease (PD) is a genetically complex disorder in which combinations of heterozygous risk variants may contribute to pathogenesis. Many PD risk loci encode lysosomal genes, such as GBA1, a common and potent risk factor, conferring at least a 5-fold increase. However, the mechanisms of GBA1 penetrance remain poorly understood.
Methods
Using Drosophila melanogaster, we performed a genetic interaction screen of lysosomal storage disorder (LSD) genes to identify dominant modifiers of Gba1b (fly homolog of GBA1). Age-dependent locomotor assessments, electroretinograms (ERG), transmission electron microscopy (TEM) analyses and quantification of dopaminergic (DA) neurons were used to assess the neurodegenerative phenotypes of double heterozygous animals.
By combining immunostaining, lipidomics, metabolomics and pharmacological approaches we showed how partial loss of anne (fly homolog of ATP13A2) and Gba1b drives neurodegeneration. By interrogating genetic data from local and international PD cohorts we identified double heterozygous pathogenic variants in ATP13A2 and GBA1 in individuals with PD.
Results
We show that anne is expressed in neurons, whereas Gba1b is expressed in glia. Flies heterozygous for anne exhibit mild neurodegenerative phenotypes, and Gba1b strongly enhances this haploinsufficiency.
Double heterozygous (Gba1bT2A/+;anneT2A/+) flies exhibit a slow and progressive neurodegeneration associated with accumulation and impaired acidification of lysosomes in photoreceptors and other neurons. Obvious morphological defects are first observed in glia at day 15 after eclosion and include vacuolization and neuronal detachment.
These defects are accompanied by an elevation of glucosylceramide (GlcCer) and followed by loss of neuronal function and degenerative features by day 30. These phenotypes are neuronal activity-dependent.
The neurodegenerative phenotypes are rescued by: ML-SA1, an agonist of the lysosomal TRPML1 channel that has been reported to promote lysosomal membrane trafficking; myriocin, a compound that inhibits GlcCer production; and DFMO, a drug which inhibits polyamine synthesis. Based on surveys of genetic data, we identify multiple PD cases harboring digenic variants in GBA1 and ATP13A2.
Conclusions
Our study reveals that partial loss of Gba1b in glia and anne in neurons synergistically disrupts lysosomal pH and neuron-glia GlcCer homeostasis, triggering neurodegeneration. Our results provide evidence that GBA1 penetrance is influenced by additional genetic modifiers, consistent with a putative digenic mechanism for GBA1-PD penetrance.
These findings highlight lysosomal acidification, sphingolipid clearance, and polyamine regulation as critical intervention points in digenic PD.