A major epidemiological registry-based study from Aarhus University and Aarhus University Hospital indicates that Parkinson’s disease begins in the gastrointestinal tract; the study is the largest in the field so far.
The chronic neurodegenerative Parkinson’s disease affects an increasing number of people. However, scientists still do not know why some people develop Parkinson’s disease. Now researchers from Aarhus University and Aarhus University Hospital have taken an important step towards a better understanding of the disease.
New research indicates that Parkinson’s disease may begin in the gastrointestinal tract and spread through the vagus nerve to the brain.
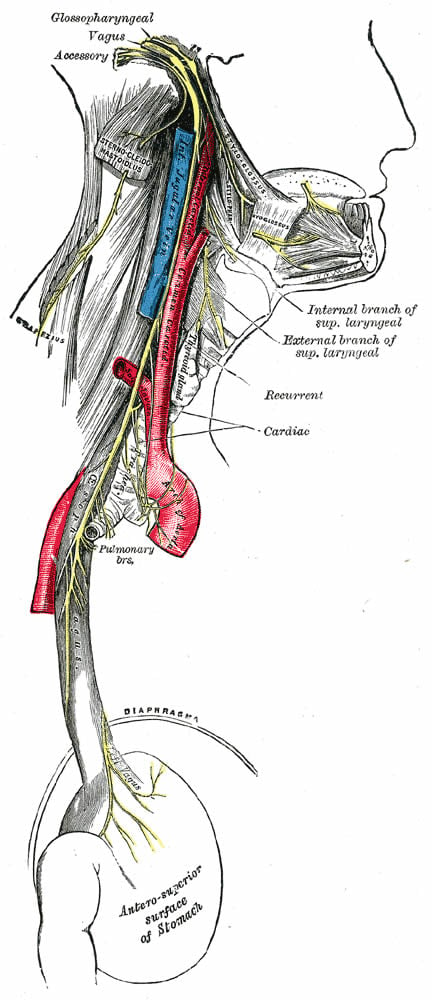
“We have conducted a registry study of almost 15,000 patients who have had the vagus nerve in their stomach severed. Between approximately 1970-1995 this procedure was a very common method of ulcer treatment. If it really is correct that Parkinson’s starts in the gut and spreads through the vagus nerve, then these vagotomy patients should naturally be protected against developing Parkinson’s disease,” explains postdoc at Aarhus University Elisabeth Svensson on the hypothesis behind the study.
A hypothesis that turned out to be correct:
“Our study shows that patients who have had the the entire vagus nerve severed were protected against Parkinson’s disease. Their risk was halved after 20 years. However, patients who had only had a small part of the vagus nerve severed where not protected. This also fits the hypothesis that the disease process is strongly dependent on a fully or partially intact vagus nerve to be able to reach and affect the brain,” she says.
The research project has just been published in the internationally recognised journal Annals of Neurology.
The first clinical examination
The research has presented strong evidence that Parkinson’s disease begins in the gastrointestinal tract and spreads via the vagus nerve to the brain. Many patients have also suffered from gastrointestinal symptoms before the Parkinson’s diagnosis is made.
“Patients with Parkinson’s disease are often constipated many years before they receive the diagnosis, which may be an early marker of the link between neurologic and gastroenterologic pathology related to the vagus nerve ,” says Elisabeth Svensson.
Previous hypotheses about the relationship between Parkinson’s and the vagus nerve have led to animal studies and cell studies in the field. However, the current study is the first and largest epidemiological study in humans.
The research project is an important piece of the puzzle in terms of the causes of the disease. In the future the researchers expect to be able to use the new knowledge to identify risk factors for Parkinson’s disease and thus prevent the disease.
“Now that we have found an association between the vagus nerve and the development of Parkinson’s disease, it is important to carry out research into the factors that may trigger this neurological degeneration, so that we can prevent the development of the disease. To be able to do this will naturally be a major breakthrough,” says Elisabeth Svensson.
Facts
- Parkinson’s disease is a chronic and neurodegenerative disease which affects approx. 1 out of every 1,000 people.
- The first signs of the disease are most often seen between the ages of 50-60.
- The researchers carried out a registry study involving 14,883 patients who had undergone a vagotomy.
- The research project was supported by the Danish Parkinson’s Disease Association and PROCRIN (Program for Clinical Research Infrastructure).
Funding The research was funded by the Danish Parkinson’s Disease Association.
Source: Elisabeth Svensson – Aarhus University
Image Credit: Image is credited to the Gray’s Anatomy and is in the public domain
Original Research: Abstract for “Vagotomy and subsequent risk of Parkinson’s disease” by Elisabeth Svensson PhD, Erzsébet Horváth-Puhó PhD, Reimar W Thomsen PhD, Jens Christian Djurhuus DMSc, Lars Pedersen PhD, Per Borghammer DMSc and Henrik Toft Sørensen DMSc in Annals of Neurology. Published online June 2015 doi:10.1002/ana.24448
Abstract
Vagotomy and subsequent risk of Parkinson’s disease
Objectives: Parkinson’s disease (PD) may be caused by an enteric neurotropic pathogen entering the brain through the vagal nerve, a process that may take over 20 years. We investigated the risk of PD in patients who underwent vagotomy, and hypothesized that truncal vagotomy is associated with a protective effect, while super-selective vagotomy has a minor effect.
Methods: We constructed cohorts of all patients in Denmark who underwent vagotomy during 1977-1995 and a matched general population cohort, by linking Danish registries. We used Cox regression to compute hazard ratios (HRs) for PD and corresponding 95% confidence intervals [CIs], adjusting for potential confounders.
Results: Risk of PD was decreased in patients who underwent truncal [HR = 0.85, 95% CI= 0.56–1.27; follow-up of >20 years: HR = 0.58, 95% CI: 0.28–1.20] compared to super-selective vagotomy. Risk of PD was also decreased following truncal vagotomy when compared to the general population cohort [overall adjusted HR = 0.85, 95% CI 0.63–1.14; follow-up >20 years, adjusted HR = 0.53 [95% CI: 0.28–0.99]. In patients who underwent super-selective vagotomy, risk of PD was similar to the general population [HR = 1.09, 95% CI: 0.84–1.43; follow-up of >20 years: HR = 1.16, 95% CI: 0.80–1.70]. The statistical precision of the risk estimates was limited. Results were consistent after external adjustment for unmeasured confounding by smoking.
Interpretation: Full truncal vagotomy is associated with a decreased risk for subsequent PD, suggesting that the vagal nerve may be critically involved in the pathogenesis of PD.
“Vagotomy and subsequent risk of Parkinson’s disease” by Elisabeth Svensson PhD, Erzsébet Horváth-Puhó PhD, Reimar W Thomsen PhD, Jens Christian Djurhuus DMSc, Lars Pedersen PhD, Per Borghammer DMSc and Henrik Toft Sørensen DMSc in Annals of Neurology. Published online June 2015 doi:10.1002/ana.24448







