Summary: CBD does not appear to reduce experimental pain intensity but does make the experience of pain less unpleasant.
Source: Syracuse University
It’s been hailed as a wonder drug and it’s certainly creating wonder profits. By some estimates, the Cannabidiol (or CBD) market could be worth $20 billion dollars by 2024. While users tout its effectiveness in pain relief, up until now there’s been limited experimental human research on the actual effectiveness of the drug.
However, a new study led by researchers at Syracuse University sheds light on the ability of CBD to reduce pain along with the impact that the so-called placebo effect may have on pain outcomes.
“For science and the public at large the question remained, is the pain relief that CBD users claim to experience due to pharmacological effects or placebo effects,” asked Martin De Vita, a researcher in the psychology department at Syracuse University’s College of Arts and Sciences.
“That’s a fair question because we know that simply telling someone that a substance has the ability to relieve their pain can actually cause robust changes in their pain sensitivity. These are called expectancy effects.”
De Vita, along with Syracuse Emeritus Psychology Professor Stephen Maisto, were uniquely prepared to answer that exact question. The pair, along with fellow lab member and doctoral candidate Dezarie Moskal, previously conducted the first systematic review and meta-analysis of experimental research examining the effects cannabinoid drugs on pain.
As the first experimental pain trial to examine CBD, their study yielded consistent and noteworthy results.
Among other findings, the data showed that CBD and expectancies for receiving CBD do not appear to reduce experimental pain intensity, but do make the pain feel less unpleasant.
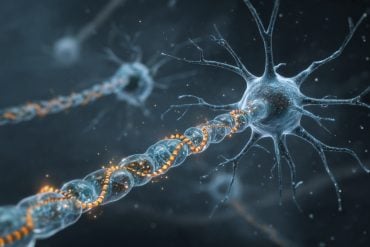
De Vita and Maisto used sophisticated equipment that safely induces experimental heat pain, allowing them to measure how the recipient’s nervous system reacts and responds to it.
“Then we administer a drug, like pure CBD, or a placebo and then re-assess their pain responses and see how they change based on which substance was administered,” said De Vita.
Researchers then took it a step farther by manipulating the information given to participants about which substances they received.
In some cases, participants were told that they got CBD when they actually received a placebo, or told they would be getting a placebo when they actually got CBD.
“That way we could parse out whether it was the drug that relieved the pain, or whether it was the expectation that they had received the drug that reduced their pain,” according to De Vita.

“We hypothesized that we would primarily detect expectancy-induced placebo analgesia (pain relief). What we found though after measuring several different pain outcomes is that it’s actually a little bit of both. That is, we found improvements in pain measures caused by the pharmacological effects of CBD and the psychological effects of just expecting that they had gotten CBD. It was pretty remarkable and surprising.”
“The data is exciting but pretty complex in that different pain measures responded differently to the drug effect, to the expectancy, or both the drug and expectancy combined—so we’re still trying to figure out what is behind the differential data with different kinds of pain measures,” said Maisto.
“The next step is studying the mechanisms underlying these findings and figuring out why giving instructions or CBD itself causes certain reactions to a pain stimulus.”
Most people think of pain as an on and off switch, you either have it or you don’t. But pain, as De Vita describes it, is a complex phenomenon with several dimensions influenced by psychological and biological factors. For example, whereas pain intensity reflects a “sensory” dimension of pain, unpleasantness represents an “affective,” or emotional, aspect of pain.
“If you think of pain as the noxious noise coming from a radio the volume can represent the intensity of the pain, while the station can represent the quality,” said De Vita. Results from his previous study showed that while cannabinoid drugs weren’t reducing the volume of pain, they were “changing the channel making it a little less unpleasant.”
According to De Vita, “It’s not sunshine and rainbows pleasant, but something slightly less bothersome. We replicated that in this study and found that CBD and expectancies didn’t significantly reduce the volume of the pain, but they did make it less unpleasant—it didn’t bother them as much.”
As part of the study De Vita and Maisto developed advanced experimental pain measurement protocols “to pop the hood and start looking at some of these other mechanistic pain processes,” said De Vita.
“It’s not just pain, yes or no, but there are these other dimensions of pain, and it would be interesting to see which ones are being targeted. We found that sometimes pharmacological effects of CBD brought down some of those, but the expectancies did not. Sometimes they both did it. Sometimes it was just the expectancy. And so, we were going into this thinking we were going to primarily detect the expectancy-induced pain relief but what we found out was way more complex than that and that’s exciting.”
One important note to also consider is the source of the CBD. “What we used in our study was pure CBD isolate oil,” said De Vita.
“Commercially available CBD products differ in their content and purity, so results might be different for different CBD products, depending on what other compounds they may or may not contain.”
About this pain and CBD research news
Source: Syracuse University
Contact: Press Office – Syracuse University
Image: The image is in the public domain
Original Research: Closed access.
“The effects of cannabidiol and analgesic expectancies on experimental pain reactivity in healthy adults: A balanced placebo design trial” by Martin J. De Vita et al. Experimental and Clinical Psychopharmacology
Abstract
The effects of cannabidiol and analgesic expectancies on experimental pain reactivity in healthy adults: A balanced placebo design trial
Despite its frequent use for pain relief, no experimental pain research has tested the analgesic effects of cannabidiol (CBD) in humans. The goal of this study was to experimentally test the effects of CBD and expectancies for receiving CBD on human pain reactivity.
Using a crossover, 2 × 2 factorial balanced placebo design, drug administration (given inactive substance or given active CBD) and verbal instruction sets (told inactive substance or told active CBD) were experimentally manipulated. Fifteen healthy adults each completed four separate experimental sessions.
Participants were randomly assigned to different counterbalanced manipulation conditions at each session: control (told inactive—given inactive); expectancy (told active CBD—given inactive); drug (told inactive—given active CBD); and expectancy + drug (told active CBD—given active CBD). Primary outcomes were pain threshold, tolerance, intensity, unpleasantness, conditioned pain modulation (CPM), and offset analgesia (OA).
There was a significant main effect of instructions on OA, such that the OA response was significantly larger when participants were told that they received CBD, regardless of drug content. Pain unpleasantness was significantly reduced in the drug, expectancy, and expectancy + drug conditions, relative to the control condition.
The drug and expectancy conditions separately improved CPM, whereas the expectancy + drug and control conditions produced the lowest CPM change scores. We did not detect significant effects for pain threshold, tolerance, or intensity.
Our results indicated that separate pain outcomes can be differentially affected by CBD and/or expectancies for receiving CBD. Future investigations of the psychological and pharmacological mechanisms underlying CBD analgesia are warranted.