Summary: Researchers believe low oxygen therapy could prevent, and may even reverse, mitochondrial disorders in people.
Source: Howard Hughes Medical Institute.
Thin air can reverse brain damage due to mitochondrial defects in mice.
After a month of breathing air that contains about half the usual amount of oxygen, telltale lesions in the brains of these mice had disappeared, Howard Hughes Medical Institute (HHMI) Investigator Vamsi Mootha and colleagues report online May 8 in the Proceedings of the National Academy of Sciences.
“We found, much to our surprise and delight, that we could actually reverse advanced disease,” Mootha says. “I don’t think anybody thought that these types of neurological diseases could be reversible.”
It’s a remarkable turnaround — though the result was seen in mice, not humans. More research is needed before a similar approach could be used to treat people, cautions Mootha, a mitochondrial biologist at Massachusetts General Hospital in Boston. Still, the findings hint at the promise of low oxygen therapy to prevent, or even reverse, mitochondrial disorders in people.
One such disorder is Leigh syndrome, a rare disease that often appears in the first few years of life. The disorder is marked by progressive brain lesions, a loss of motor skills, developmental delays and a failure to grow. Most forms of the disease have no proven treatments.
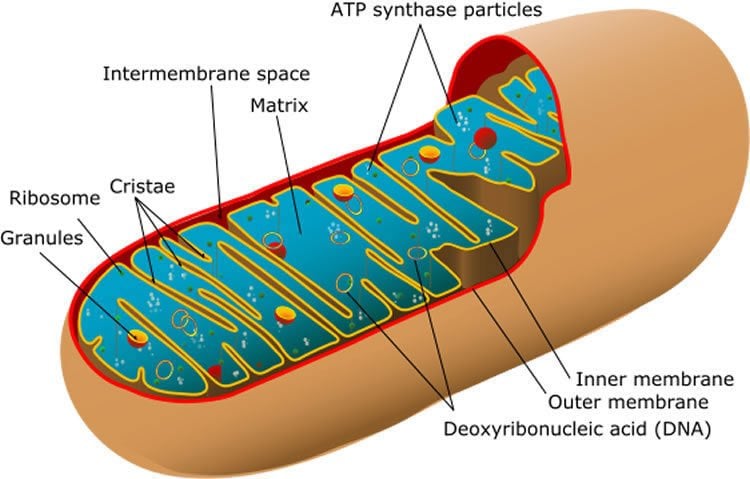
Yet Mootha and his team had what seems like a counterintuitive idea. In 2016, the researchers reported that hypoxia, or oxygen deficiency, actually improves the health of mice genetically engineered to have dysfunctional mitochondria, tiny power-producing organelles. Those results, published in Science, were tantalizing, and also raised a number of questions, such as how long these treated mice actually live, and whether hypoxia treatment needs to be continuous.
The new findings answer some of these questions. “At a high level, this is exploring the remarkable potential and also the limitations of hypoxia,” Mootha says.
The mice in the study were genetically engineered to lack a gene called Ndufs4, which encodes a protein essential for a part of mitochondria called complex I. That same gene is mutated in some people with Leigh syndrome.
When these mice were housed in chambers that contained normal air containing 21 percent oxygen, the equivalent of what a person would breathe at sea level, they developed brain lesions and had a median survival length of 58 days. But when these mice were kept in chambers that contained 11 percent oxygen, their median survival time stretched to 270 days, Mootha and colleagues found. What’s more, MRI images revealed these mice had no signs of abnormally bright brain tissue, lesions that often signal degeneration.
Eleven percent oxygen is close to what a person would encounter at high altitudes such as the base camp at Mount Everest. “Is it super comfortable? Certainly not,” Mootha says, but a healthy person would be able to tolerate it.
Based on his team’s earlier work, Mootha wasn’t surprised that the mice treated with hypoxia lived longer. But a different result was unexpected: A switch to hypoxic conditions seemed to actually reverse existing brain damage. After a month of breathing low oxygen air, lesions in the mices’ brains disappeared, MRI images revealed.
While the results in the mice are “profound and striking,” Mootha emphasizes that the research is still at an early stage. Much more work needs to be done before hypoxia can be used to treat people with mitochondria disorders. “We are not ready yet to go into the clinic,” he says.
Other results help illustrate remaining hurdles to developing a hypoxia therapy. Mootha and his team had hoped to find benefits for more moderate low-oxygen conditions, such as intermittent periods of hypoxia or slightly higher levels of oxygen. But so far, the results suggest that only continuous 11 percent oxygen does the trick. “The disappointing part was that we didn’t come up with a more practical regimen, at least in this paper,” Mootha says.
Still, he and his team plan to keep looking for other ways to get the hypoxia benefits without the intense hypoxia conditions, perhaps with a small molecule. The researchers also plan to study how exactly the hypoxia response works — how low-oxygen conditions kindle molecular efforts to protect and repair the brain.
The results have implications that stretch beyond mitochondrial diseases. Neurodegenerative disorders that have been associated with aging, and even normal aging, have been linked to a diminished mitochondrial power. “As all of us age, our mitochondrial activity declines,” Mootha says. Hypoxia, or a drug that mimics a key aspect of it, might one day be able to rejuvenate flagging mitochondria, and perhaps the aging body, too.
Funding: Funding provided by Howard Hughes Medical Institute, Marriott Mitochondrial Disorders Research Fund, US Department of Energy.
Source: Meghan Rosen – Howard Hughes Medical Institute
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Full open access research for “Hypoxia treatment reverses neurodegenerative disease in a mouse model of Leigh syndrome” by Michele Ferrari, Isha H. Jain, Olga Goldberger, Emanuele Rezoagli, Robrecht Thoonen, Kai-Hung Chen, David E. Sosnovik, Marielle Scherrer-Crosbie, Vamsi K. Mootha, and Warren M. Zapol in Human Molecular Genetics. Published online May 8 2017 doi:10.1073/pnas.1621511114
[cbtabs][cbtab title=”MLA”]Howard Hughes Medical Institute “Low Oxygen Reverses Mitochondrial Disease: Mouse Study.” NeuroscienceNews. NeuroscienceNews, 8 May 2017.
<https://neurosciencenews.com/oxygen-mitochondrial-disease-6618/>.[/cbtab][cbtab title=”APA”]Howard Hughes Medical Institute (2017, May 8). Low Oxygen Reverses Mitochondrial Disease: Mouse Study. NeuroscienceNew. Retrieved May 8, 2017 from https://neurosciencenews.com/oxygen-mitochondrial-disease-6618/[/cbtab][cbtab title=”Chicago”]Howard Hughes Medical Institute “Low Oxygen Reverses Mitochondrial Disease: Mouse Study.” https://neurosciencenews.com/oxygen-mitochondrial-disease-6618/ (accessed May 8, 2017).[/cbtab][/cbtabs]
Abstract
Hypoxia treatment reverses neurodegenerative disease in a mouse model of Leigh syndrome
The most common pediatric mitochondrial disease is Leigh syndrome, an episodic, subacute neurodegeneration that can lead to death within the first few years of life, for which there are no proven general therapies. Mice lacking the complex I subunit, Ndufs4, develop a fatal progressive encephalopathy resembling Leigh syndrome and die at ≈60 d of age. We previously reported that continuously breathing normobaric 11% O2 from an early age prevents neurological disease and dramatically improves survival in these mice. Here, we report three advances. First, we report updated survival curves and organ pathology in Ndufs4 KO mice exposed to hypoxia or hyperoxia. Whereas normoxia-treated KO mice die from neurodegeneration at about 60 d, hypoxia-treated mice eventually die at about 270 d, likely from cardiac disease, and hyperoxia-treated mice die within days from acute pulmonary edema. Second, we report that more conservative hypoxia regimens, such as continuous normobaric 17% O2 or intermittent hypoxia, are ineffective in preventing neuropathology. Finally, we show that breathing normobaric 11% O2 in mice with late-stage encephalopathy reverses their established neurological disease, evidenced by improved behavior, circulating disease biomarkers, and survival rates. Importantly, the pathognomonic MRI brain lesions and neurohistopathologic findings are reversed after 4 wk of hypoxia. Upon return to normoxia, Ndufs4 KO mice die within days. Future work is required to determine if hypoxia can be used to prevent and reverse neurodegeneration in other animal models, and to determine if it can be provided in a safe and practical manner to allow in-hospital human therapeutic trials.
“Hypoxia treatment reverses neurodegenerative disease in a mouse model of Leigh syndrome” by Michele Ferrari, Isha H. Jain, Olga Goldberger, Emanuele Rezoagli, Robrecht Thoonen, Kai-Hung Chen, David E. Sosnovik, Marielle Scherrer-Crosbie, Vamsi K. Mootha, and Warren M. Zapol in Human Molecular Genetics. Published online May 8 2017 doi:10.1073/pnas.1621511114






