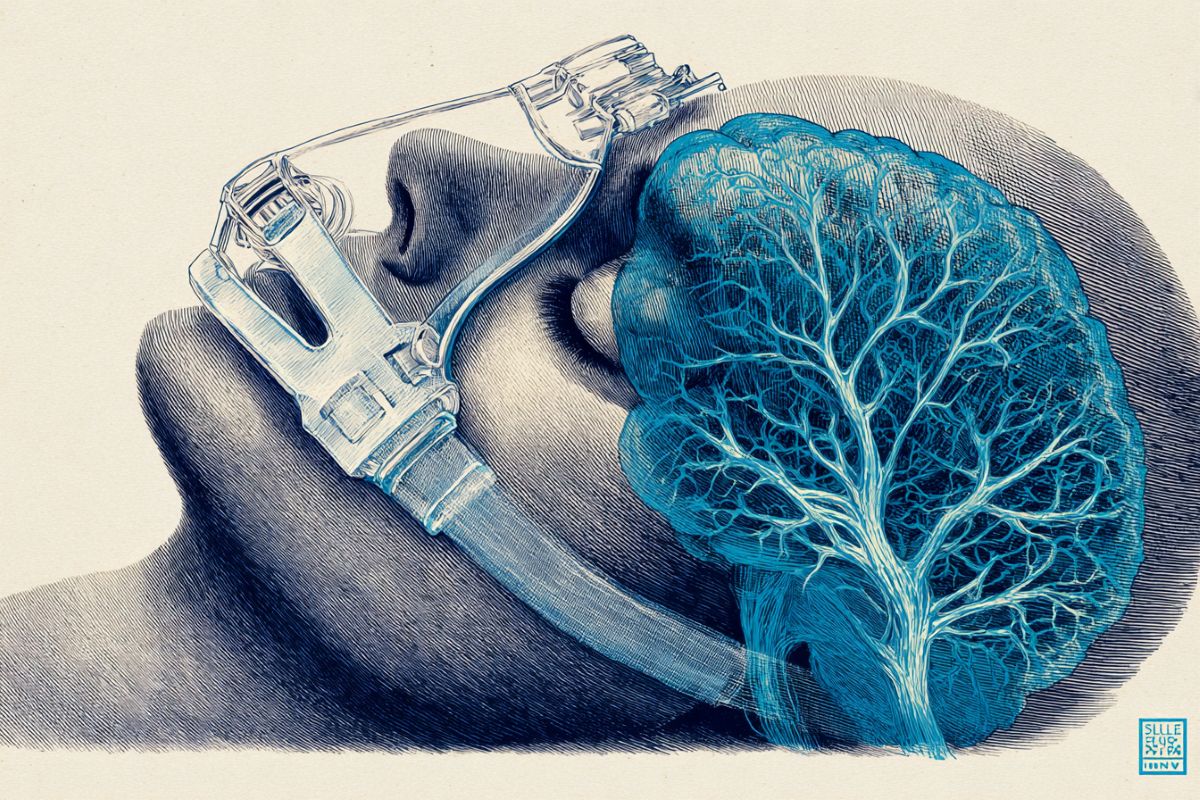
Summary: A large analysis of more than 11 million medical records found that people with untreated obstructive sleep apnea face a substantially higher risk of developing Parkinson’s disease over time. Even after accounting for factors like age, obesity, and cardiovascular conditions, those who did not use CPAP were nearly twice as likely to be diagnosed with Parkinson’s as those who treated their apnea.
The findings highlight how repeated nighttime drops in oxygen may heighten long-term vulnerability of the brain’s neural circuits. Researchers say the results underscore the importance of sleep-quality interventions as a potential buffer against neurodegenerative disease.
Key Facts:
- Higher Risk: Untreated sleep apnea nearly doubled long-term Parkinson’s risk compared to treated apnea.
- Protective CPAP: Regular CPAP use significantly reduced the likelihood of developing Parkinson’s.
- Oxygen Stress: Chronic oxygen disruption during sleep may predispose neurons to degeneration.
Source: Oregon Health and Science University
New research reveals that people with untreated obstructive sleep apnea have a higher risk of developing Parkinson’s disease. However, they can significantly reduce the risk by improving the quality of their sleep by using continuous positive airway pressure, or CPAP.
The study, which published today in the journal JAMA Neurology, examined electronic health records covering more than 11 million U.S. military veterans who received care through the Department of Veterans Affairs between 1999 and 2022.
The research was led by Oregon Health & Science University and the Portland VA Health Care System.
Parkinson’s is a neurodegenerative condition that affects an estimated 1 million people nationwide, with the risk rising incrementally year by year for people over age 60.
The new study suggests a heightened risk of people with untreated sleep apnea developing Parkinson’s over the long term.
Even after adjusting to rule out confounding factors like obesity, age and high blood pressure, the study found a strong link between untreated sleep apnea and Parkinson’s. Among millions of people with sleep apnea, those who didn’t treat the condition with CPAP were nearly twice as likely to have Parkinson’s as those who did.
“It’s not at all a guarantee that you’re going to get Parkinson’s, but it significantly increases the chances,” said co-author Gregory Scott, M.D., Ph.D., assistant professor of pathology in the OHSU School of Medicine and a pathologist for at the VA Portland.
Sleep apnea is a common condition where an individual’s breathing stops and restarts many times during sleep, which can prevent the body from getting enough oxygen.
“If you stop breathing and oxygen is not at a normal level, your neurons are probably not functioning at a normal level either,” said lead author Lee Neilson, M.D., assistant professor of neurology at OHSU and a staff neurologist at the Portland VA.
“Add that up night after night, year after year, and it may explain why fixing the problem by using CPAP may build in some resilience against neurodegenerative conditions, including Parkinson’s.”
Neilson said he intends to prioritize the health benefits of sound sleep with his patients, especially in view of the research revealing an elevated risk of Parkinson’s.
“I think it will change my practice,” he said.
Scott noted that even though some people with sleep apnea resist treatment with CPAP, he pointed to the experience of many veterans who swear by it.
“The veterans who use their CPAP love it,” he said. “They’re telling other people about it. They feel better, they’re less tired. Perhaps if others know about this reduction in risk of Parkinson’s disease, it will further convince peopel with sleep apnea to give CPAP a try.”
In addition to Scott and Neilson, co-authors include Isabella Montano, B.A., Jasmin May, M.D., Ph.D., Jonathan Elliott, Ph.D., and Miranda Lim, M.D., Ph.D., of OHSU and the Portland VA Health Care System; and Yeilim Cho, M.D., and Jeffrey Iliff, Ph.D., of the University of Washington and the VA Puget Sound Health Care System.
Funding: The research was supported by the VA, grant awards BX005760, CX00253, I01RX004822, I01RX005371, CX002022, BX006155 and Bx006155; the John and Tami Marick Family Foundation, the Collins Medical Trust; the National Institute on Aging of the National Institutes of Health, award P30AG066518; and the U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick, Maryland 21702-5014, under award numbers HT9425-24-1-0774 and HT9425-24-1-0775.
Opinions, interpretations, conclusions and recommendations are those of the authors and are not necessarily endorsed by the Department of Defense, the NIH, VA or other funders.
Key Questions Answered:
A: Yes, people with untreated sleep apnea were nearly twice as likely to develop Parkinson’s.
A: Yes, consistent CPAP use significantly reduced Parkinson’s risk in long-term data.
A: Chronic oxygen disruption may harm neurons over years, increasing vulnerability to disease.
Editorial Notes:
- This article was edited by a Neuroscience News editor.
- Journal paper reviewed in full.
- Additional context added by our staff.
About this sleep apnea and Parkinson’s disease research news
Author: Erik Robinson
Source: Oregon Health and Science University
Contact: Erik Robinson – Oregon Health and Science University
Image: The image is credited to Neuroscience News
Original Research: Closed access.
“Obstructive Sleep Apnea, Positive Airway Pressure, and Implications of Early Treatment in Parkinson Disease” by Gregory Scott et al. JAMA Neurology
Abstract
Obstructive Sleep Apnea, Positive Airway Pressure, and Implications of Early Treatment in Parkinson Disease
Importance
Obstructive sleep apnea (OSA) is associated with many health conditions, including dementia and early mortality. Prior epidemiological studies linking OSA with Parkinson disease (PD) are conflicting, and no studies have examined the influence of continuous positive airway pressure (CPAP), the criterion standard treatment for OSA, on PD risk.
Objective
To examine the association between OSA with incident Parkinson disease among US veterans and risk modification by CPAP.
Design, Setting, and Participants
This electronic health record (EHR)–based cohort study was conducted among US veterans from January 1, 1999, to December 30, 2022, with mean (SD) follow-up of 4.9 (1.8) years. Veterans with PD at the time of exposure or incomplete records were excluded. Data analysis was completed from September 2024 to September 2025.
Exposure
OSA was defined by its appropriate administrative code; CPAP usage was extracted from a semistructured medical interview field in the EHR.
Main Outcomes and Measures
The primary outcome, cumulative incidence of PD, was calculated adjusting for competing risk of death after balancing for age, race, sex, and smoking status.
Results
A total of 13 737 081 US veterans were screened, and 11 310 411 veterans (1 109 543 female veterans [9.8%]) with mean (SD) age of 60.5 (14.7) years were included in analyses. Of included veterans, 1 552 505 (13.7%) had OSA. Veterans with OSA demonstrated 1.61 additional cases of PD (point estimate; 95% CI, 1.13-2.09) at 6 years from diagnosis per 1000 people compared to those without OSA.
Results were confirmed when adjusting for body mass index, vascular comorbidities, psychiatric conditions, and relevant medications and were of greater magnitude in female veterans. Case numbers were significantly reduced when treated with CPAP early in the disease course.
Conclusions and Relevance
In this EHR-based cohort study, OSA appeared to be an independent risk factor for the later development of PD and could be modified by early treatment with CPAP. Effective screening measures and protocols for consistent adherence to CPAP may have large impacts on brain health.