A new study from researchers at UH Rainbow Babies and Children’s Hospital and other centers suggests that preterm infants with a low-grade bleeding in the brain may have similar neurodevelopmental outcomes as infants with no bleeding. The study appears online at JAMA Pediatrics.
The study’s lead author Allison Payne, MD MS, a neonatologist at UH Rainbow Babies and Children’s Hospital and instructor at Case Western Reserve University School of Medicine, said, “The results are important because it is a large multi-center study showing different results than a recent study that did find differences in outcomes at 2 years of age for babies with PIVH. Our study’s results are similar to those reported by other international cohorts.”
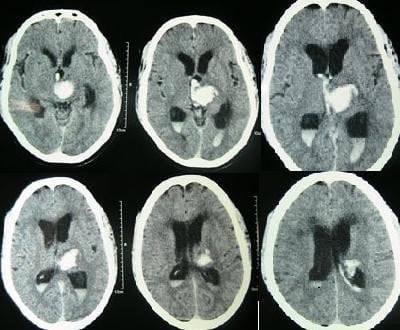
The bleeding is called periventricular-intraventricular hemorrhage (PIVH), a condition that can occur in preterm babies. Dr. Payne and her colleagues said that although the presence of severe PIVH strongly correlates with adverse motor and cognitive outcomes, “outcomes of survivors with low-grade PIVH (grade 1 or 2) are less fully understood despite accounting for 50 percent to 80 percent of all PIVH cases.”

In this study, the researchers analyzed 1472 extremely preterm infants admitted to 16 pediatric medical centers, including UH Rainbow Babies and Children’s Hospital, from 2006 to 2008 who survived to 18-22 months and had at least one cranial ultrasonography performed during their stay.
In total, 451 infants were diagnosed with PIVH, of which 31 percent were classified as having grade 1 PIVH, 29 percent as having grade 2, and 40 percent as having grade 3 or 4. Infants with grade 1 or 2 PIVH did not have an increased incidence of poor neurodevelopmental outcomes at 18-22 months compared with infants without PIVH, even after multivariate analysis controlling for potential confounders, including the use of antenatal and postnatal steroids.
Compared with low-grade hemorrhage, severe (grade 3 or 4) hemorrhage was significantly associated with cognitive deficits and language delay, as well as an increased risk for poor nonsensory outcomes (including cerebral palsy) apart from mild language impairment and severe cognitive impairment.
The researchers caution that high-prevalence, low-severity disabilities, such as attention deficit/hyperactivity disorders, specific neuropsychological deficits, and behavioral problems may gradually emerge over the years. “It is not clear what contribution low-grade PIVH may have to these more subtle disabilities,” said Dr. Payne. She plans to continue to study these children when they reach school age.
Notes about this neurodevelopment research
Other authors on the paper from UH Rainbow Babies and Children’s Hospital are Anna Maria Hibbs, MD, MS; Michele C. Walsh, MD, MS, and Deanne E. Wilson-Costello, MD. The research was supported by the National Institutes of Health (NIH) and Rainbow Babies and Children’s Foundation Fellowship Research Award Program. NIH; Eunice Kennedy Shriver National Institute of Child Health and Human Development; National Center for Research Resources, and National Center for Advancing Translational Sciences provided grant support for the Neonatal Research Network’s Generic Database and Follow-up Studies.
Contact: George Stamatis – University Hospitals Case Medical Center
Source: University Hospitals Case Medical Center press release
Image Source: The CT scan of intracerebral hemorrhage image is credited to Yadav YR, Mukerji G, Shenoy R, Basoor A, Jain G, Nelson A at Wikimedia Commons and is licensed as Creative Commons Attribution 2.0 Generic.
Original Research: Abstract for “Neurodevelopmental Outcomes of Extremely Low-Gestational-Age Neonates With Low-Grade Periventricular-Intraventricular Hemorrhage” by Allison H. Payne, MD, MS; Susan R. Hintz, MD, MS; Anna Maria Hibbs, MD, MS; Michele C. Walsh, MD, MS; Betty R. Vohr, MD; Carla M. Bann, PhD and Deanne E. Wilson-Costello, MD in JAMA Pediatrics. Published online March 4 2013 doi:10.1001/jamapediatrics.2013.866