Research could have direct application for treating human drinking problems.
A research team led by scientists from the Ernest Gallo Clinic and Research Center at the University of California, San Francisco has identified circuitry in the brain that drives compulsive drinking in rats, and likely plays a similar role in humans.
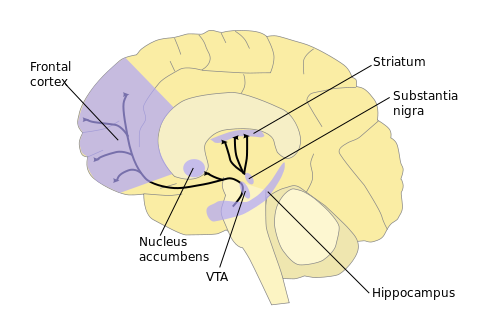
The scientists found they could reduce compulsive drinking in rats by inhibiting key neural pathways that run between the prefrontal cortex, which is involved with higher functions such as critical thinking and risk assessment, and the nucleus accumbens, a critical area for reward and motivation.
The authors noted that there are already several FDA-approved medications that target activity in these pathways, thus potentially opening an accelerated track to new treatments for compulsive drinking.
The study describing their finding was published online on June 30 in Nature Neuroscience.
The study was conducted on rats that regularly drank 20 percent alcohol. The rats drank both unmixed alcohol and alcohol mixed with extremely bitter quinine, said senior investigator F. Woodward Hopf, PhD, an assistant adjunct professor of neurology at UCSF.

Hopf explained that this alcohol-quinine solution, which he described as “like a vodka tonic without the sugar,” is often used as a rodent model of compulsive drinking, or “drinking in the face of negative consequences.” In rats, he said, the negative consequence is the bitter taste, while in humans who drink compulsively, “the negative consequences are profound: people continue to drink despite the potential loss of jobs, marriages, freedom, even their lives.”
In the United States, alcoholism is estimated to cost $224 billion per year – almost $2 per drink – mostly from lost productivity and crime, and leads to 100,000 preventable deaths per year.
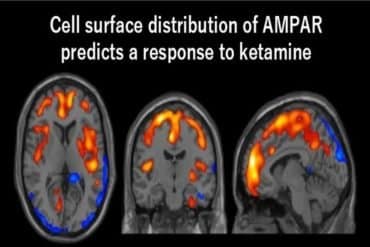
The drinking rats showed a notable increase in the NMDA receptor (NMDAR), which lead author Taban Seif, PhD, a Gallo Center researcher, called “a molecule that excites the brain.” When the rats were injected with an NMDAR blocker, their consumption of quinine-laced alcohol dropped significantly, while regular alcohol use was unaffected. “In other words, only the compulsive drinking was affected,” said Seif.
The team then focused its research on connections from two specific regions of the rats’ prefrontal cortex where they had discovered the presence of unusual types of NMDARs: the medial prefrontal cortex, which mediates conflict during decision-making, and the insula, which is critical for self-awareness and feelings. “In a non-addict, these brain areas tell you when something is potentially harmful and bad, and to run away as fast as possible,” said Hopf. “But if you’re a compulsive drinker, it seems instead that they give you a comforting pat on the back, in effect telling you it’s OK to have another drink, nothing to worry about.”
Using a technique called optogenetics, the scientists inserted halorhodopsin, a light-sensitive protein, into these areas. They then used fiber-optic cables implanted in the rats’ brains to send pulses of laser light that activated the halorhodopsin, which in turn inhibited the regions’ connections to the nucleus accumbens. The researchers found that rats inhibited in this way drank significantly less quinine-laced alcohol, while their intake of regular alcohol solution remained unaffected.
“The fact that we reduced the rats’ compulsive drinking using two different methods – an NMDAR blocker and direct inhibition of connections – tells us that we have probably identified the right areas,” said Hopf.
The next logical step for the research team, said Hopf, would be to work with clinical researchers on an NMDAR blocker trial in human subjects.
“What is interesting is that we have a new drug which could perhaps treat compulsive aspects of drinking,” said Hopf, “but only if you are in conflict about your drinking – if you care. Any therapy with NMDAR blockers would need a strong behavioral and cognitive component to make sure the patient stayed mentally engaged.”
Seif and Hopf also plan further experimental studies focusing on how the insula drives behavior and connects to other areas of the brain.
Notes about this neurology and alcoholism research
Co-authors of the paper are Shao-Ju Chang, Jeffrey A Simms, Stuart L. Gibb, PhD, and Jahan Dadgar of the Gallo Center; Billy T. Chen, PhD, and Brandon K. Harvey of the National Institute on Drug Abuse; Dorit Ron, PhD, of the Gallo Center and UCSF; Robert O. Messing, MD, of the Gallo Center and UCSF at the time of the research and currently of the University of Texas at Austin; and Antonello Bonci, MD, of the Gallo Center, UCSF and the Johns Hopkins University, Baltimore, MD.
The study was supported by funds from the National Institute on Alcohol Abuse and Alcoholism, the National Institute on Drug Abuse and the State of California through UCSF.
Contact: Jeffrey Norris – UCSF
Source: UCSF press release
Image Source: The brain image is credited to NIDA/Quasihuman and is in the public domain.
Original Research: Abstract for “Cortical activation of accumbens hyperpolarization-active NMDARs mediates aversion-resistant alcohol intake” by Taban Seif, Shao-Ju Chang, Jeffrey A Simms, Stuart L Gibb, Jahan Dadgar, Billy T Chen, Brandon K Harvey, Dorit Ron, Robert O Messing, Antonello Bonci and F Woodward Hopf in Nature Neuroscience. Published online June 30 2013 doi:10.1038/nn.3445