Summary: Living in disadvantaged neighborhoods not only influences food choices and weight gain but can also alter the brain’s microstructure.
Researchers found that poor food quality, high-calorie intake, and inactive environments common in such areas disrupt brain regions crucial for emotion, cognition, and reward processing. A direct link was established between brain cortex changes and high trans-fatty acid intake, prevalent in such neighborhoods.
These findings emphasize the urgent need to improve dietary quality in deprived areas for better brain health.
Key Facts:
- Disadvantaged neighborhoods can lead to changes in the brain’s cortex related to reward, emotion, and cognition due to poor dietary habits.
- The study included 92 participants and used advanced MRI scans to study the brain structure in relation to the Area Deprivation Index (ADI).
- High intake of trans-fatty acids from foods, common in these neighborhoods, directly impacted specific areas of the brain’s cortex.
Source: UCLA
You are what you eat, according to the adage. But it’s not just the body that’s impacted. According to research from UCLA David Geffen School of Medicine, living in a disadvantaged neighborhood can affect food choices, weight gain and even the microstructure of the brain.
The study, appearing in Communications Medicine, finds poor quality of available foods, increased intake of calories from foods high in trans-fatty acids, and environments that do not foster physical activity, all prevalent in disadvantaged neighborhoods, disrupt the flexibility of information processing in the brain that is involved in reward, emotion regulation, and cognition.
Previous research showed that living in a disadvantaged neighborhood can impact brain health, but in this study, researchers did a detailed analysis of the brain’s cortex to determine how living in a disadvantaged area can change specific areas of the brain that play different roles.
“We found that neighborhood disadvantage was associated with differences in the fine structure of the cortex of the brain. Some of these differences were linked to higher body mass index and correlated with high intake of the trans-fatty acids found in fried fast food,” said Arpana Gupta, PhD, co-Director of the Goodman-Luskin Center and Director of the Neuroimaging Core.
“Our results suggest that regions of the brain involved in reward, emotion, and the acquisition of knowledge and understanding might be affected by aspects of neighborhood disadvantage that contribute to obesity,” said Gupta, senior author. “This highlights the importance of addressing dietary quality issues in disadvantaged neighborhoods to protect brain health.”
Neighborhood disadvantage is defined by a combination of such factors as low median income, low education level, crowding, and lack of complete plumbing.
This study included 92 participants – 27 men and 65 women – from the greater Los Angeles area. Demographic and body mass index information was collected, and neighborhood disadvantage was assessed as to its area deprivation index (ADI) using University of Wisconsin School of Medicine’s Public Health’s Neighborhood Atlas.
Earlier studies have found that people living in disadvantaged neighborhoods are at higher risk of obesity due to the poor quality of available foods, increased intake of calories from foods high in trans-fatty acids, and environments that do not foster physical activity.
In this study, researchers focused on the relationship between ADI and neuroimaging results at four levels of the brain cortex to investigate in more refined detail the connections between neighborhood disadvantage and brain structure. Participants underwent two types of MRI scans that, when analyzed in combination, provide insights into brain structure, signaling and function.
“Different populations of cells exist in different layers of the cortex, where there are different signaling mechanisms and information-processing functions,” said Lisa Kilpatrick, PhD, a researcher in the Goodman-Luskin Microbiome Center focusing on brain signatures related to brain-body dysregulation, the study’s first author.
“Examining the microstructure at different cortical levels provides a better understanding of alterations in cell populations, processes and communication routes that may be affected by living in a disadvantaged neighborhood.”
According to the results, worse ADI ratings were associated with communication changes in brain regions that are important for social interaction. Other changes occurred in regions involved in reward, emotion regulation, and higher cognitive processes – and these changes appeared to be affected by trans-fatty acid intake.
Together, the findings suggest that factors prevalent in disadvantaged neighborhoods that encourage poor diet and unhealthy weight gain “disrupt the flexibility of information processing involved in reward, emotion regulation, and cognition.”
Authors Gupta and Kilpatrick are both corresponding authors. Other authors, all from UCLA, include Keying Zhang, Tien Dong, Gilbert Gee, Hiram Beltran-Sanchez, May Wang, Jennifer Labus, Bruce Naliboff and Emeran Mayer.
Funding This research was supported by grants from the National Institutes of Health, including R01 MD015904 (AG), K23 DK106528 (AG), R03 DK121025 (AG), T32 DK07180 (TD), ULTR001881/DK041301 (UCLA CURE/CTSI Pilot and Feasibility Study (AG), R01 DK048351 (EAM), P30 DK041301; and pilot funds provided for brain scanning by the Ahmanson-Lovelace Brain Mapping Center. These funders played no role in study design, or the collection, analysis, and interpretation of the data.
About this neuroscience and psychology research news
Author: David Sampson
Source: UCLA
Contact: David Sampson – UCLA
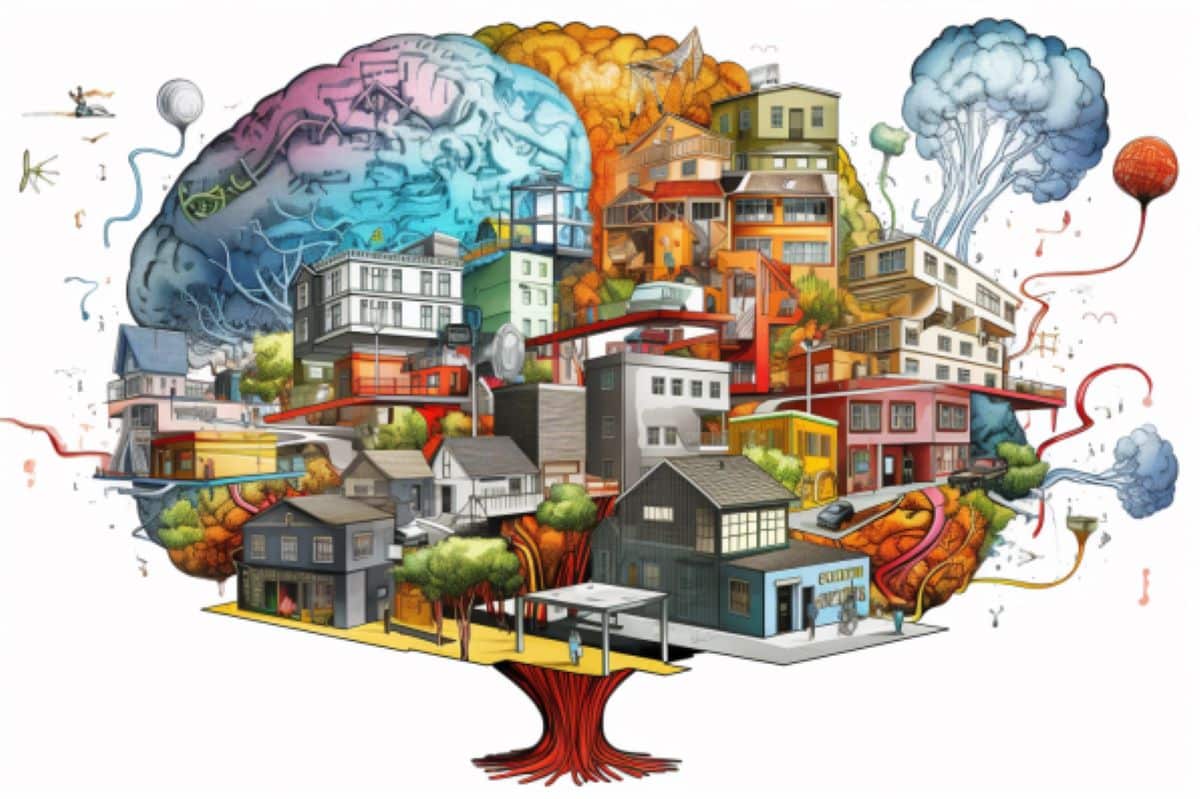
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Mediation of the association between disadvantaged neighborhoods and cortical microstructure by body mass index” by Arpana Gupta et al. Communications Medicine
Abstract
Mediation of the association between disadvantaged neighborhoods and cortical microstructure by body mass index
Background
Living in a disadvantaged neighborhood is associated with worse health outcomes, including brain health, yet the underlying biological mechanisms are incompletely understood. We investigated the relationship between neighborhood disadvantage and cortical microstructure, assessed as the T1-weighted/T2-weighted ratio (T1w/T2w) on magnetic resonance imaging, and the potential mediating roles of body mass index (BMI) and stress, as well as the relationship between trans-fatty acid intake and cortical microstructure.
Methods
Participants comprised 92 adults (27 men; 65 women) who underwent neuroimaging and provided residential address information. Neighborhood disadvantage was assessed as the 2020 California State area deprivation index (ADI). The T1w/T2w ratio was calculated at four cortical ribbon levels (deep, lower-middle, upper-middle, and superficial). Perceived stress and BMI were assessed as potential mediating factors. Dietary data was collected in 81 participants.
Results
Here, we show that worse ADI is positively correlated with BMI (r = 0.27, p = .01) and perceived stress (r = 0.22, p = .04); decreased T1w/T2w ratio in middle/deep cortex in supramarginal, temporal, and primary motor regions (p < .001); and increased T1w/T2w ratio in superficial cortex in medial prefrontal and cingulate regions (p < .001). Increased BMI partially mediates the relationship between worse ADI and observed T1w/T2w ratio increases (p = .02). Further, trans-fatty acid intake (high in fried fast foods and obesogenic) is correlated with these T1w/T2w ratio increases (p = .03).
Conclusions
Obesogenic aspects of neighborhood disadvantage, including poor dietary quality, may disrupt information processing flexibility in regions involved in reward, emotion regulation, and cognition. These data further suggest ramifications of living in a disadvantaged neighborhood on brain health.