Summary: Researchers developed tiny “mini-brains” from stem cells to help diagnose and treat Alzheimer’s disease. These mini-brains, created from human blood, accurately reflect the pathology of Alzheimer’s on a smaller scale. This innovative technology could revolutionize healthcare, especially for remote communities, by providing a simpler way to diagnose neurological conditions.
Key Facts:
- Innovative Approach: “Mini-brains” are built from stem cells and mimic human brain pathology.
- Diagnostic Potential: They could provide a new method for diagnosing Alzheimer’s and other neurological conditions.
- Healthcare Impact: This technology could benefit remote communities by enabling diagnoses from blood samples.
Source: University of Saskatchewan
Using an innovative new method, a University of Saskatchewan (USask) researcher is building tiny pseudo-organs from stem cells to help diagnose and treat Alzheimer’s.
When Dr. Tyler Wenzel (PhD) first came up with the idea of building a miniature brain from stem cells, he never could have predicted how well his creations would work.
Now, Wenzel’s “mini-brain” could revolutionize the way Alzheimer’s and other brain-related diseases are diagnosed and treated.
“Never in our wildest dreams did we think that our crazy idea would work,” he said. “These could be used as a diagnostic tool, built from blood.”
Wenzel, a postdoctoral fellow in the College of Medicine’s Department of Psychiatry, developed the idea for the “mini-brain” – or more formally, a one-of-a-kind cerebral organoid model – while working under the supervision of Dr. Darrell Mousseau (PhD).
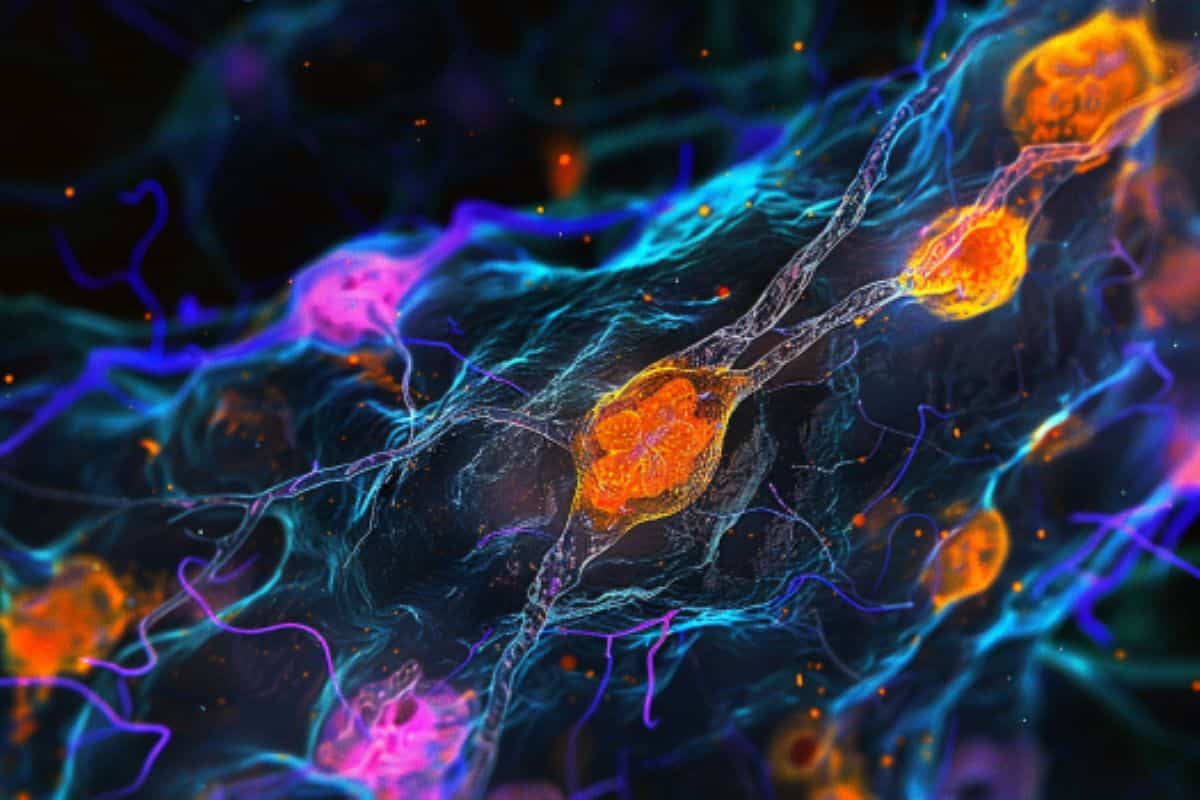
Human stem cells can be manipulated to develop into practically any other cell in the body. Using stem cells taken from human blood, Wenzel was able to create a tiny artificial organ – roughly three millimetres across and resembling visually what Wenzel described as a piece of chewed gum someone has tried to smooth out again.
These “mini-brains” are built by creating stem cells from a blood sample, and then transforming these stem cells into functioning brain cells. Using small synthetic organoids for research is not a novel concept – but the “mini-brains” developed in Wenzel’s lab are unique.
As outlined in Wenzel’s recent published article in Frontiers of Cellular Neuroscience, the brains from Wenzel’s lab are comprised of four different types of brain cells while most brain organoids are comprised of only neurons.
In testing, Wenzel’s “mini-brains” more accurately reflect a fully-fledged adult human brain, so they can be used to more closely examine neurological conditions of adult patients, such as Alzheimer disease.
And for those “mini-brains” created from the stem cells of individuals who have Alzheimer’s, Wenzel determined that the artificial organ displayed the pathology of Alzheimer’s – just on a smaller scale.
“If stem cells have the capacity to become any cell in the human body, the question then came ‘could we create something that resembles an entire organ?’” Wenzel said.
“While we were developing it, I had the crazy idea that if these truly are human brains, if a patient had a disease like Alzheimer’s and we grew their ‘mini-brain,’ in theory that tiny brain would have Alzheimer’s.”
Wenzel said this technology has the potential to change the way health services are provided to those with Alzheimer’s, particularly in rural and remote communities. This groundbreaking research has already received support from the Alzheimer Society of Canada.
If Wenzel and his colleagues can create a consistent way to diagnose and treat neurological conditions like Alzheimer’s using only a small blood sample – which has a relatively long shelf life and can be couriered – instead of requiring patients to travel to hospitals or specialized clinics, it could be a tremendous resource savings for the healthcare system and a burden off of patients.
“In theory, if this tool works the way we think it does, we could just get a blood sample shipped from La Loche or La Ronge to the university and diagnose you like that,” he said.
The early proof-of-concept work on the “mini-brains” has been extremely promising – which means the next step for Wenzel is expanding the testing to a larger pool of patients.
The researchers are also interested in trying to expand the scope of the “mini-brain” research. According to Wenzel, if they can confirm the “mini-brains” accurately reflect other brain diseases or neurological conditions, they could potentially be used to speed up diagnoses or test the efficacy of drugs on patients.
As an example, Wenzel pointed to the substantial wait times to see a psychiatrist in Saskatchewan. If the “mini-brains” could be used to test which antidepressant works best on a patient suffering from depression, it could dramatically reduce the time required to see a doctor and receive a prescription.
A former high school science teacher who made the move into the world of research and academia, Wenzel said it’s the “nature of research” to come up with a hypothesis and hit close to the mark in an experiment that excites him his work.
The astounding success of the early “mini-brains,” however, has been so staggering that Wenzel admitted he still struggles to wrap his own brain around it.
“I’m still in disbelief, but it’s also extremely motivating that something like this happened,” Wenzel said.
“It gives me something that I think will impact society and have actual relevance and create some change … it has a strong potential to shift the landscape of medicine.”
About this neurology and Alzheimer’s research news
Author: Daniel Hallen
Source: University of Saskatchewan
Contact: Daniel Hallen – University of Saskatchewan
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Brain organoids engineered to give rise to glia and neural networks after 90 days in culture exhibit human-specific proteoforms” by Tyler Wenzel et al. Frontiers in Cellular Neuroscience
Abstract
Brain organoids engineered to give rise to glia and neural networks after 90 days in culture exhibit human-specific proteoforms
Human brain organoids are emerging as translationally relevant models for the study of human brain health and disease.
However, it remains to be shown whether human-specific protein processing is conserved in human brain organoids.
Herein, we demonstrate that cell fate and composition of unguided brain organoids are dictated by culture conditions during embryoid body formation, and that culture conditions at this stage can be optimized to result in the presence of glia-associated proteins and neural network activity as early as three-months in vitro.
Under these optimized conditions, unguided brain organoids generated from induced pluripotent stem cells (iPSCs) derived from male–female siblings are similar in growth rate, size, and total protein content, and exhibit minimal batch-to-batch variability in cell composition and metabolism.
A comparison of neuronal, microglial, and macroglial (astrocyte and oligodendrocyte) markers reveals that profiles in these brain organoids are more similar to autopsied human cortical and cerebellar profiles than to those in mouse cortical samples, providing the first demonstration that human-specific protein processing is largely conserved in unguided brain organoids.
Thus, our organoid protocol provides four major cell types that appear to process proteins in a manner very similar to the human brain, and they do so in half the time required by other protocols.
This unique copy of the human brain and basic characteristics lay the foundation for future studies aiming to investigate human brain-specific protein patterning (e.g., isoforms, splice variants) as well as modulate glial and neuronal processes in an in situ-like environment.