Summary: Researchers have identified a crucial biochemical mechanism that could allow Huntington’s disease to be studied before symptoms appear, offering hope for early intervention. The team found that disrupted dopamine regulation in specific neurons, related to TrkB neurotrophin receptor signaling, may trigger Huntington’s onset. By targeting an enzyme called GSTO2, researchers prevented motor symptoms in a mouse model, suggesting this protein’s role in the disease’s progression.
The discovery opens avenues for developing early diagnostic tests and preventive treatments to maintain dopamine balance. This breakthrough could ultimately delay or halt Huntington’s devastating effects, particularly by addressing biochemical changes before irreversible brain damage occurs.
Key Facts:
- Disrupted TrkB signaling in iSPNs leads to dopamine imbalance linked to Huntington’s symptoms.
- Enzyme GSTO2 plays a role in dopamine regulation; reducing its activity delayed HD symptoms in mice.
- Early intervention on this biochemical pathway may help prevent disease progression before symptoms appear.
Source: Oxford University
Researchers from the University of Oxford have identified a key biochemical mechanism relevant to the development of Huntington’s Disease. This discovery opens up the possibility of studying the disease before its clinical onset and eventually stopping its progression.
The study, published in Nature Metabolism, has shown for the first time the biochemical change responsible for the development of Huntington’s disease, and how blocking this change stopped disease progression.
Huntington’s disease is an inherited condition that stops parts of the brain from working properly, leading to mental and physical decline that slowly worsens over time. The symptoms usually begin to appear after the age of 30 years and are fatal, but this can be after a period of up to 20 years, during which they worsen.
The study explores how an early change described in the brain of HD patients in the early 1980s could lead to Huntington’s disease onset.
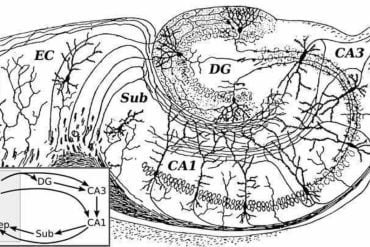
The researchers identified that problems with specific neurons in the brain, called indirect pathway spiny projection neurons (iSPNs), which are the initially affected cells in HD, may trigger an imbalance in dopamine levels upon missing an important signalling derived from the activation of the neurotrophin receptor TrkB.
This imbalance is linked to early symptoms of the disease, such as abnormal, involuntary movements.
First the researchers looked at mice that lacked normal function in these iSPNs due to disrupted TrkB neurotrophin signalling and noticed that they showed increased levels of dopamine in the brain, leading to hyperactivity.
This change occurred before noticeable symptoms appeared, suggesting that these early alterations may contribute significantly to HD progression.
The researchers also found that a protein called GSTO2, an enzyme that is part of the glutathione metabolism, plays an important role in regulating dopamine levels. By selectively reducing the activity of this protein in mice, the researchers were able to prevent dopamine and energy metabolism dysfunction, arresting the onset of motor symptoms in mice.
Importantly, this enzyme shows similar dysregulation in a rat model of HD and some rare brains of asymptomatic HD patients, confirming its putative relevance to the development of the disorder.
The study’s lead author, Liliana Minichiello, Professor of Cellular and Molecular Neuroscience at Oxford’s Department of Pharmacology, said: ‘The big problem with Huntington’s disease is that by the time that symptoms develop much of the damage has already been done, and therefore, it is fundamental that we understand the changes that occur before the disorder develops if we are to develop effective therapeutics.’
‘This research marks the first time that we have been able to identify a specific chemical change that is unique to the development of Huntington’s disease, which opens the possibility of developing new tests to study the early changes of the disease before irreversible damage occurs.
‘Understanding these early changes provides crucial insights into how Huntington’s Disease develops, and this knowledge could help develop preventive therapies to maintain dopamine balance and delay or halt disease progression.’
Dr Yaseen Malik (Department of Pharmacology, Oxford University), first author of the paper, said: ‘Despite our significant understanding of its pathophysiology, HD remains without a cure, which underscores the necessity of delivering diagnostic and therapeutic interventions prior to the onset of symptoms, and this study is a step in that direction.’
About this Huntington’s disease research news
Author: Caroline Wood
Source: Oxford University
Contact: Caroline Wood – Oxford University
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Impaired striatal glutathione–ascorbate metabolism induces transient dopamine increase and motor dysfunction” by Liliana Minichiello et al. Nature Metabolism
Abstract
Impaired striatal glutathione–ascorbate metabolism induces transient dopamine increase and motor dysfunction
Identifying initial triggering events in neurodegenerative disorders is critical to developing preventive therapies.
In Huntington’s disease (HD), hyperdopaminergia—probably triggered by the dysfunction of the most affected neurons, indirect pathway spiny projection neurons (iSPNs)—is believed to induce hyperkinesia, an early stage HD symptom. However, how this change arises and contributes to HD pathogenesis is unclear.
Here, we demonstrate that genetic disruption of iSPNs function by Ntrk2/Trkb deletion in mice results in increased striatal dopamine and midbrain dopaminergic neurons, preceding hyperkinetic dysfunction.
Transcriptomic analysis of iSPNs at the pre-symptomatic stage showed de-regulation of metabolic pathways, including upregulation of Gsto2, encoding glutathione S-transferase omega-2 (GSTO2). Selectively reducing Gsto2 in iSPNs in vivo effectively prevented dopaminergic dysfunction and halted the onset and progression of hyperkinetic symptoms.
This study uncovers a functional link between altered iSPN BDNF-TrkB signalling, glutathione–ascorbate metabolism and hyperdopaminergic state, underscoring the vital role of GSTO2 in maintaining dopamine balance.