Summary: A new study reports people with Hepatitis B are upto 76% more likely to develop Parkinson’s disease, and those with Hep C are 51% more likely to develop the disease.
Source: AAN.
The viruses hepatitis B and C may both be associated with an increased risk of Parkinson’s disease, according to a study published in the March 29, 2017, online issue of Neurology. The hepatitis virus affects the liver.
According to the Centers for Disease Control and Prevention (CDC), it is estimated that anywhere from 850,000 to 2.2 million people in the United States have chronic hepatitis B virus infection and anywhere from 2.7 to 3.9 million people have chronic hepatitis C. While both can lead to serious illness, many people have few symptoms and do not realize they have the virus, especially at first.
Hepatitis B is spread through contact with blood and body fluids of an infected person, such as unprotected sex, sharing needles, getting a tattoo or piercing with unsterilized tools or sharing razors or toothbrushes with an infected person.
Hepatitis C is spread through blood-to-blood contact such as sharing needles, razors and toothbrushes and is passed on at birth by infected mothers.
“The development of Parkinson’s disease is complex, with both genetic and environmental factors,” said study author Julia Pakpoor, BM, BCh, of the University of Oxford in the United Kingdom. “It’s possible that the hepatitis virus itself or perhaps the treatment for the infection could play a role in triggering Parkinson’s disease or it’s possible that people who are susceptible to hepatitis infections are also more susceptible to Parkinson’s disease. We hope that identifying this relationship may help us to better understand how Parkinson’s disease develops.”
For the study, researchers examined hospital records from a large British database. They looked for records of people with a first case of hepatitis B, hepatitis C, autoimmune hepatitis, chronic active hepatitis and HIV from 1999 to 2011. Then those people were compared to the hospital records of people with relatively minor conditions such as cataract surgery, bunions and knee replacement surgery. For all of the participants, researchers looked at the records to see who later developed Parkinson’s disease.
There were nearly 22,000 people with hepatitis B, 48,000 with hepatitis C, 6,000 with autoimmune hepatitis, 4,000 with chronic active hepatitis and nearly 20,000 with HIV. They were compared to more than 6 million people with minor conditions.
The study found that people with hepatitis B were 76 percent more likely to develop Parkinson’s disease than those in the comparison group, and people with hepatitis C were 51 percent more likely to develop Parkinson’s disease. A total of 44 people with hepatitis B developed Parkinson’s disease, compared to 25 cases that would be expected in the general population. For people with hepatitis C, 73 people developed Parkinson’s disease, where about 49 cases would have been expected in the general population.
People with autoimmune hepatitis, chronic active hepatitis and HIV did not have an increased rate of Parkinson’s disease.
A previous study from Taiwan showed a relationship between hepatitis C and Parkinson’s disease, but it did not show any relationship for hepatitis B.
Pakpoor said that limitations of the current study include that they could not adjust for lifestyle factors such as smoking and alcohol use, which could affect Parkinson’s disease risk, and that the study was based solely on people who were evaluated at a hospital.
Funding: The British National Institute for Health Research funded the development of the datasets and software.
Source: Renee Tessman – AAN
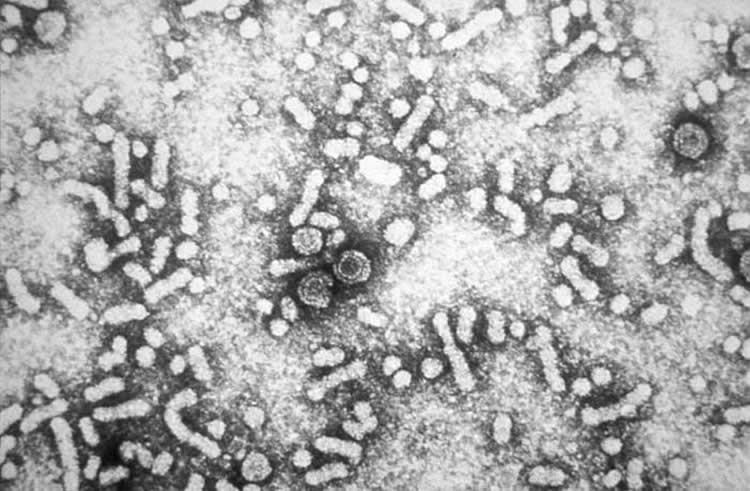
Image Source: NeuroscienceNews.com image is credited to CDC.
Original Research: Abstract for “Viral hepatitis and Parkinson disease” by Julia Pakpoor, BA, BM BCh*, Alastair Noyce, MRCP, PhD*, Raph Goldacre, MSc, Marianna Selkihova, MRCP, PhD, Stephen Mullin, BSc, MRCP, Anette Schrag, FRCP, PhD, Andrew Lees, FRCP, MD and Michael Goldacre, FFPH, FRCP in AAN Computational Biology. Published online March 29 2017 doi:10.1212/WNL.0000000000003848
[cbtabs][cbtab title=”MLA”]AAN “Hepatitis B and C May Be Linked to Increased Risk of Parkinson’s Disease.” NeuroscienceNews. NeuroscienceNews, 31 March 2017.
<https://neurosciencenews.com/hepatitis-b-c-parkinsons-6318/>.[/cbtab][cbtab title=”APA”]AAN (2017, March 31). Hepatitis B and C May Be Linked to Increased Risk of Parkinson’s Disease. NeuroscienceNew. Retrieved March 31, 2017 from https://neurosciencenews.com/hepatitis-b-c-parkinsons-6318/[/cbtab][cbtab title=”Chicago”]AAN “Hepatitis B and C May Be Linked to Increased Risk of Parkinson’s Disease.” https://neurosciencenews.com/hepatitis-b-c-parkinsons-6318/ (accessed March 31, 2017).[/cbtab][/cbtabs]
Abstract
Viral hepatitis and Parkinson disease
Objective: To study associations between viral hepatitis and Parkinson disease (PD).
Methods: A retrospective cohort study was done by analyzing linked English National Hospital Episode Statistics and mortality data (1999–2011). Cohorts of individuals with hepatitis B, hepatitis C, autoimmune hepatitis, chronic active hepatitis, and HIV were constructed, and compared to a reference cohort for subsequent rates of PD.
Results: The standardized rate ratio (RR) of PD following hepatitis B was 1.76 (95% confidence interval [CI] 1.28–2.37) (p < 0.001), based on 44 observed compared with 25 expected cases. The RR of PD following hepatitis C was 1.51 (95% CI, 1.18–1.9) (p < 0.001), based on 48.5 expected and 73 observed cases. There was no significant association between autoimmune hepatitis, chronic active hepatitis or HIV, and subsequent PD. When including only those episodes of care for PD that occurred first at least 1 year following each exposure condition, the RR for hepatitis B and hepatitis C were 1.82 (1.29–2.5) and 1.43 (1.09–1.84), respectively. Conclusions: We report strong evidence in favor of an elevation of rates of subsequent PD in patients with hepatitis B and hepatitis C. These findings may be explained by factors peculiar to viral hepatitis, but whether it reflects consequences of infection, shared disease mechanisms, or the result of antiviral treatment remains to be elucidated. Further work is needed to confirm this association and to investigate pathophysiologic pathways, potentially advancing etiologic understanding of PD more broadly.
“Viral hepatitis and Parkinson disease” by Julia Pakpoor, BA, BM BCh, Alastair Noyce, MRCP, PhD, Raph Goldacre, MSc, Marianna Selkihova, MRCP, PhD, Stephen Mullin, BSc, MRCP, Anette Schrag, FRCP, PhD, Andrew Lees, FRCP, MD and Michael Goldacre, FFPH, FRCP in AAN Computational Biology. Published online March 29 2017 doi:10.1212/WNL.0000000000003848






