Summary: Researchers report appetite signals cross a single synapse in under 100 milliseconds, relaying information from the gut to the brain much quicker than previously thought.
Source: Duke University.
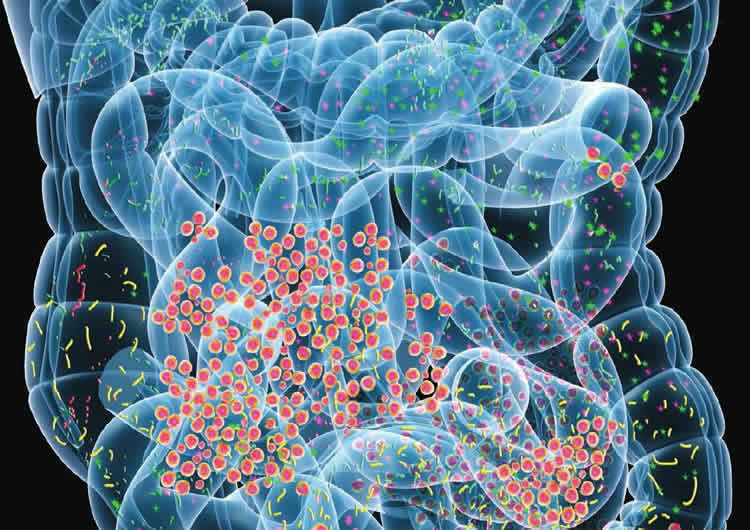
If you’ve ever felt nauseous before an important presentation, or foggy after a big meal, then you know the power of the gut-brain connection.
Scientists now believe that a surprising array of conditions, from appetite disorders and obesity to arthritis and depression, may get their start in the gut. But it hasn’t been clear how messages in this so-called “second brain” spread from our stomachs to our cerebrum. For decades, researchers believed that hormones in the bloodstream were the indirect channel between the gut and the brain.
Recent research suggests the lines of communication behind that “gut feeling” is more direct and speedy than a diffusion of hormones. Using a rabies virus jacked up with green fluorescence, Duke researchers traced a signal as it traveled from the intestines to the brainstem of mice. They were shocked to see the signal cross a single synapse in under 100 milliseconds — that’s faster than the blink of an eye.
“Scientists talk about appetite in terms of minutes to hours. Here we are talking about seconds,” said Diego Bohórquez, Ph.D., senior author of the study and assistant professor of medicine at Duke University School of Medicine. “That has profound implications for our understanding of appetite. Many of the appetite suppressants that have been developed target slow-acting hormones, not fast-acting synapses. And that’s probably why most of them have failed.”
The research appears Sept. 21 in the journal Science.
Your brain takes in information from all five senses — touch, sight, hearing, smell and taste — through electrical signals, which travel along long nerve fibers that lie beneath your skin and muscle like fiber optic cables. These signals move fast, which is why the scent of freshly baked cookies seems to hit you the moment you open a door.
Though the gut is just as important a sensory organ as your eyes and ears — after all, knowing when your stomach is in need of a fill-up is key to survival — scientists thought it delivered its messages by a multi-step, somewhat indirect process. Nutrients in your gut, the thinking went, stimulated the release of hormones, which entered the bloodstream minutes to hours after eating, eventually exerting their effects on the brain.
They were partly right. That tryptophan in your turkey dinner is notorious for its transformation into serotonin, the brain chemical that makes you feel sleepy.
But Bohórquez suspected the brain had a way of perceiving cues from the gut more quickly. He noticed that the sensory cells lining the gut shared many of the same characteristics as their cousins on the tongue and in the nose. In 2015, he published a landmark study in the Journal of Clinical Investigation showing that these gut cells contained nerve endings or synapses, suggesting that they might tap into some kind of neural circuitry.
In this study, Bohórquez and his team set out to map that circuitry. First, postdoctoral fellow Maya Kaelberer pumped a rabies virus carrying a green fluorescent tag into the stomachs of mice. She saw that the virus had labeled the vagus nerve before landing in the brainstem, showing her there was a direct circuit.
Next, Kaelberer recreated the gut-brain neural circuit by growing sensory gut cells of mice in the same dish with vagal neurons. She saw the neurons crawl along the surface of the dish to connect to the gut cells and begin to fire signals. When the research team added sugar to the mix, the firing rate sped up. Kaelberer measured how fast the information from sugar in the gut was communicated and was shocked to find it was on the order of milliseconds.
That finding suggested that a neurotransmitter like glutamate — which is involved in conveying other senses like smell and taste — might act as the messenger. Sure enough, when the researchers blocked the release of glutamate in the sensory gut cells, the messages were silenced.
Bohórquez has data that suggests the structure and function of this circuit will be the same in humans.
“We think these findings are going to be the biological basis of a new sense,” Bohórquez said. “One that serves as the entry point for how the brain knows when the stomach is full of food and calories. It brings legitimacy to idea of the ‘gut feeling’ as a sixth sense.”
In the future, Bohórquez and his team are interested in figuring out how this new sense can discern the type of nutrients and caloric value of the foods we eat.
Funding: This research was supported by the National Institutes of Health (K01DK-103832, R03DK114500-01, P30DK034987, 1OT2023849-01), an AGA-Elsevier Pilot Research Award, a UNC Center for Gastrointestinal Biology and Disease Research Award, the Defense Advanced Research Projects Agency (ElectRxN2002850300), the Hartwell Foundation, the Dana Foundation, the Grass Foundation and the Howard Hughes Medical Institute.
Source: Karl Bates – Duke University
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Abstract for “A gut-brain neural circuit for nutrient sensory transduction” by Melanie Maya Kaelberer, Kelly L. Buchanan, Marguerita E. Klein, Bradley B. Barth, Marcia M. Montoya, Xiling Shen, and Diego V. Bohórquez in Science. Published September 21 2018.
doi:10.1126/science.aat5236
[cbtabs][cbtab title=”MLA”]Duke University”‘Gut Sense’ is Hardwired, Not Hormonal.” NeuroscienceNews. NeuroscienceNews, 21 September 2018.
<https://neurosciencenews.com/hard-wired-gut-sense-9897/>.[/cbtab][cbtab title=”APA”]Duke University(2018, September 21). ‘Gut Sense’ is Hardwired, Not Hormonal. NeuroscienceNews. Retrieved September 21, 2018 from https://neurosciencenews.com/hard-wired-gut-sense-9897/[/cbtab][cbtab title=”Chicago”]Duke University”‘Gut Sense’ is Hardwired, Not Hormonal.” https://neurosciencenews.com/hard-wired-gut-sense-9897/ (accessed September 21, 2018).[/cbtab][/cbtabs]
Abstract
A gut-brain neural circuit for nutrient sensory transduction
In 1853, Sydney Whiting wrote in his classic Memoirs of a Stomach, “…and between myself and that individual Mr. Brain, there was established a double set of electrical wires, by which means I could, with the greatest ease and rapidity, tell him all the occurrences of the day as they arrived, and he also could impart to me his own feelings and impressions.” Historically, it is known that the gut must communicate with the brain, but the underlying neural circuits and transmitters mediating gut-brain sensory transduction still remain unknown. In the gut, there is a single layer of epithelial cells separating the lumen from the underlying tissue. Dispersed within this layer reside electrically excitable cells termed enteroendocrine cells, which sense ingested nutrients and microbial metabolites. Like taste or olfactory receptor cells, enteroendocrine cells fire action potentials in the presence of stimuli. However, unlike other sensory epithelial cells, no synaptic link between enteroendocrine cells and a cranial nerve has been described. The cells are thought to act on nerves only indirectly through the slow endocrine action of hormones, like cholecystokinin. Despite its role in satiety, circulating concentrations of cholecystokinin peak only several minutes after food is ingested and often after the meal has ended. Such a discrepancy suggests that the brain perceives gut sensory cues through faster neuronal signaling. Using a mouse model, we sought to identify the underpinnings of this neural circuit that transduces a sense from gut to brain.
RATIONALE
Our understanding of brain neural circuits is being propelled forward by the emergence of molecular tools that have high topographical and temporal precision. We adapted them for use in the gut. Single-cell quantitative real-time polymerase chain reaction and single-cell Western blot enabled the assessment of synaptic proteins. A monosynaptic rabies virus revealed the neural circuit’s synapse. The neural circuit was recapitulated in vitro by using nodose neurons cocultured with either minigut organoids or purified enteroendocrine cells. This system, coupled to optogenetics and whole-cell patch-clamp recording, served to determine the speed of transduction. Whole-nerve electrophysiology, along with optical excitation and silencing, helped to uncover the neurotransmission properties of the circuit in vivo. The underlying neurotransmitter was revealed by using receptor pharmacology and a fluorescent reporter called iGluSnFR.
RESULTS
Single-cell analyses showed that a subset of enteroendocrine cells contains presynaptic adhesion proteins, including some necessary for synaptic adhesion. Monosynaptic rabies tracing revealed that enteroendocrine cells synapse with vagal nodose neurons. This neuroepithelial circuit connects the intestinal lumen with the brainstem in one synapse. In coculture, this connection was sufficient to transduce a sugar stimulus from enteroendocrine cells to vagal neurons. Optogenetic activation of enteroendocrine cells elicited excitatory postsynaptic potentials in connected nodose neurons within milliseconds. In vivo recordings showed that enteroendocrine cells are indeed necessary and sufficient to transduce a sugar stimulus to the vagus. By using iGluSnFR, we found that enteroendocrine cells synthesize the neurotransmitter glutamate, and pharmacological inactivation of cholecystokinin and glutamate receptors revealed that these cells use glutamate as a neurotransmitter to transduce fast, sensory signals to vagal neurons.
CONCLUSION
We identified a type of gut sensory epithelial cell that synapses with vagal neurons. This cell has been referred to as the gut endocrine cell, but its ability to form a neuroepithelial circuit calls for a new name. We term this gut epithelial cell that forms synapses the neuropod cell. By synapsing with the vagus nerve, neuropod cells connect the gut lumen to the brainstem. Neuropod cells transduce sensory stimuli from sugars in milliseconds by using glutamate as a neurotransmitter. The neural circuit they form gives the gut the rapidity to tell the brain of all the occurrences of the day, so that he, too, can make sense of what we eat.






