Summary: A new study supports the hypothesis that people with focal epilepsy are more susceptible to mood disorders, such as depression and anxiety.
Source: Rutgers University.
From the time of Hippocrates, physicians have suspected a link between epilepsy and depression. Now, for the first time, scientists at Rutgers University-New Brunswick and Columbia University have found evidence that seizures and mood disorders such as depression may share the same genetic cause in some people with epilepsy, which may lead to better screening and treatment to improve patients’ quality of life.
The scientists studied dozens of unusual families with multiple relatives who had epilepsy, and compared the family members’ lifetime prevalence of mood disorders with that of the U.S. population.
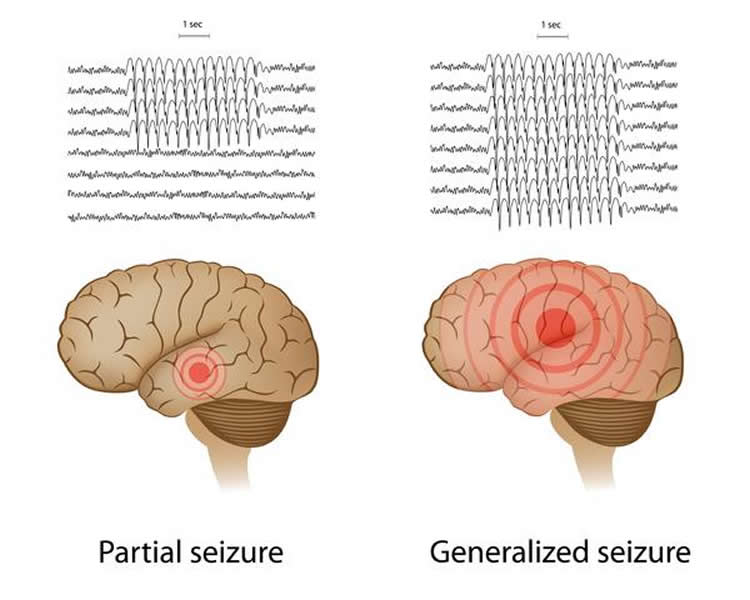
They found an increased incidence of mood disorders in persons who suffer from a type of the condition called focal epilepsy, in which seizures begin in just one part of the brain. But mood disorders were not increased in people with generalized epilepsy, in which seizures start on both sides of the brain.
“Mood disorders such as depression are under-recognized and undertreated in people with epilepsy,” said Gary A. Heiman, the study’s senior author and associate professor in the Department of Genetics at Rutgers-New Brunswick. “Clinicians need to screen for mood disorders in people with epilepsy, particularly focal epilepsy, and clinicians should treat the depression in addition to the epilepsy. That will improve patients’ quality of life.”
The results of the study – published online today in the journal Epilepsia – support the hypothesis that people with focal epilepsy, but not generalized epilepsy, are susceptible to mood disorders such as depression.
“More research is needed to identify specific genes that raise risk for both epilepsy and mood disorders,” said Heiman, who works in the School of Arts and Sciences. “It’s important to understand the relationship between the two different disorders.”
A relationship between epilepsy and mood disorders has been suspected for millennia, Heiman noted. Hippocrates, “the father of medicine,” wrote about it around 400 BC: “Melancholics ordinarily become epileptics, and epileptics, melancholics: what determines the preference is the direction the malady takes; if it bears upon the body, epilepsy, if upon the intelligence, melancholy.”
Seizures in most people with epilepsy can be controlled by drugs and surgery. The fact remains, however, that epilepsy and mood disorders such as depression affect quality of life and increase disability and healthcare costs. Depression raises the risk for suicidal thoughts and attempts. Moreover, previous studies have shown that people who have both epilepsy and mood disorders tend to have worse seizure outcomes than those without mood disorders.
In the U.S., about 2.3 million adults and more than 450,000 children and adolescents have epilepsy, and anyone can develop the disorder. In 2015, an estimated 16.1 million adults at least 18 years old in the U.S. had at least one major depressive episode in the past year, according to federal figures.
“A number of genes have been found for epilepsy and understanding if these genes also might be causing depression is important,” Heiman said. “In particular, more studies should be done to understand the relationship between focal epilepsy and mood disorders.”
Funding: Epilepsy Foundation, NIH/National Institute of Neurological Disorders and Stroke, National Institutes of Health funded this study.
Source: Todd B. Bates – Rutgers University
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is credited to the NIH.
Original Research: Abstract for “Mood disorders in familial epilepsy: A test of shared etiology” by Beverly J. Insel, Ruth Ottman, and Gary A. Heiman in Epilepsia. Published online January 10 2018 doi:10.1111/epi.13985
[cbtabs][cbtab title=”MLA”]Rutgers University “Epileptic Seizures and Depression May Share Common Genetic Cause.” NeuroscienceNews. NeuroscienceNews, 10 January 2018.
<https://neurosciencenews.com/genetics-epilepsy-depression-8297/>.[/cbtab][cbtab title=”APA”]Rutgers University (2018, January 10). Epileptic Seizures and Depression May Share Common Genetic Cause. NeuroscienceNews. Retrieved January 10, 2018 from https://neurosciencenews.com/genetics-epilepsy-depression-8297/[/cbtab][cbtab title=”Chicago”]Rutgers University “Epileptic Seizures and Depression May Share Common Genetic Cause.” https://neurosciencenews.com/genetics-epilepsy-depression-8297/ (accessed January 10, 2018).[/cbtab][/cbtabs]
Abstract
Mood disorders in familial epilepsy: A test of shared etiology
Objective
Mood disorders are the most common comorbid conditions in epilepsy, but the cause remains unclear. One possible explanation is a shared genetic susceptibility to epilepsy and mood disorders. We tested this hypothesis by evaluating lifetime prevalence of mood disorders in relatives with and without epilepsy in families containing multiple individuals with epilepsy, and comparing the findings with rates from a general population sample.
Methods
The Composite International Diagnostic Interview was administered to 192 individuals from 60 families, including 110 participants with epilepsy of unknown cause (50 focal epilepsy [FE], 42 generalized epilepsy [GE], 6 FE and GE, 12 unclassifiable) and 82 relatives without epilepsy (RWOE). Odds ratios (ORs) for lifetime prevalence of mood disorders in participants with versus without epilepsy were computed through logistic regression, using generalized estimation equations to account for familial clustering. Standardized prevalence ratios (SPRs) were used to compare prevalence in family members with general population rates.
Results
Compared with RWOE, ORs for mood disorders were significantly increased in participants with FE (OR = 2.4, 95% confidence interval [CI] = 1.1-5.2) but not in those with GE (OR = 1.0, 95% CI = 0.4-2.2). In addition, prevalence of mood disorders was increased in individuals with epilepsy who had ≥1 relative with FE. Compared with general population rates, mood disorders were significantly increased in individuals with FE but not in those with GE. Rates were also increased in RWOE, but not significantly so (SPR = 1.4, P = .14).
Significance
These findings are consistent with the hypothesis of shared genetic susceptibility to epilepsy and mood disorders, but suggest (1) the effect may be restricted to FE, and (2) the shared genetic effect on risk of mood disorders and epilepsy may be restricted to individuals with epilepsy, that is, to those in whom the genetic risk for epilepsy is “penetrant.”
“Mood disorders in familial epilepsy: A test of shared etiology” by Beverly J. Insel, Ruth Ottman, and Gary A. Heiman in Epilepsia. Published online January 10 2018 doi:10.1111/epi.13985







