Summary: New research warns that fecal microbiota transplants (FMT) can lead to long-lasting mismatches in gut regions, causing metabolic and behavioral shifts. While FMT aims to restore gut health by transplanting stool microbes from healthy donors, most microbes come from the colon and may colonize unintended regions like the small intestine.
This misplacement leads to “terraforming,” where microbes change tissue environments to suit their survival. The study urges caution and proposes a new approach—omni-microbial transplants—that better aligns microbes with their native gut environments.
Key Facts:
- Microbial Mismatch: Colon microbes from FMT can colonize unintended gut regions like the small intestine, altering function.
- Long-Term Effects: A single FMT caused persistent changes in metabolism, immune activity, and behavior in mice.
- New Proposal: Researchers suggest omni-microbial transplants to match microbes with appropriate intestinal regions.
Source: University of Chicago
Fecal microbiota transplants (FMT) have been touted as a potential treatment for a variety of conditions, from inflammatory bowel diseases, obesity, and type 2 diabetes to autism.
New research from the University of Chicago, however, cautions against widespread use of FMT because of the potential for long-lasting, unintended health consequences for recipients.
FMT involves transferring microbes in the stool from a healthy person to a sick one, in hopes of restoring a healthy equilibrium in the gut microbiome. Since stools contain primarily anaerobic microbes from the colon (i.e. they can’t tolerate oxygen), FMT can cause mismatches in the gut ecosystem when those bacteria colonize the small intestine and other parts of the digestive system.
In experiments with mice and studies with human tissue samples, the researchers conducting the new study saw that anaerobic microbes from the colon not only colonized the small bowel after a single transplant but also persisted there for months.
These microbes also changed their new intestinal environments to their advantage, “terraforming” them in ways that caused changes in the recipient’s metabolism, behavior, and energy balance.
“I think it’s a bit of a wakeup call to the field that maybe we shouldn’t willy-nilly put large bowel microbes into different parts of the intestine that shouldn’t be there,” said Orlando (Landon) DeLeon, PhD, a postdoctoral researcher at UChicago and lead author of the new study, which was published in Cell.
“If we’re designing good therapeutics, we should be aware of the importance of matching the regional microbiota to their proper environments, so that we provide better overall health benefits.”
A vast and varied ecosystem
FMT is approved by the Food and Drug Administration only for treating repeated infections with Clostridium difficile (C. diff), an opportunistic bacterium that often causes severe gastrointestinal symptoms and inflammation in hospital patients who have been on antibiotics. Seeing the success in treating C. diff patients, many physicians have been eager to use FMT to treat other digestive conditions.
Researchers understand that gut microbiome health can impact all vital organs and systems of the body, so the idea is that replacing a “sick” gut microbiome with a “healthy” one could fix the problem in one fell swoop.
The gut isn’t simply one consistent environment with the same microbiota throughout, however; instead, it has several distinct regions that are vastly different microbial ecosystems, each tailored for specific microbes that can provide functions vital to the health of their host.
“There are microbes along the entire intestinal tract, and we just study predominately the last third of it (the colon),” DeLeon said.
“So, how can you expect an FMT, with microbes from a third of the intestinal tract at the end of it, to fix the rest of the intestine?”
To test the effects of FMT on different parts of the intestine, DeLeon, Eugene B. Chang, MD, the Martin Boyer Professor of Medicine at UChicago and senior author of the study, and their team carried out a series of experiments with mice.
One group of mice was given a transplant of microbes taken from the jejunum, the first portion of the small intestine. A second group was given a standard FMT, and a third group was given a transplant from the cecum, a section connecting the small and large intestine, which has a mixture of microbes from both.
Recipients of FMT are usually treated with antibiotics first to clear out the microbes living in the gut, leaving a clean slate for newly transplanted microbes to take up residence – sometimes, however, in the wrong places.
Testing showed that microbes from each of these transplants successfully colonized the entirety of the intestinal tract in the mice, not just their native niches. This created regional gut mismatches persisting up to three months after just one transplant.
The altered microbiomes also changed the production of metabolites in each intestinal region, which can have health effects on the host. The researchers saw changes in liver metabolism, including activity in genes associated with immune function.
They also observed differences in eating behaviors, activity, and energy expenditure in the mice after transplants.
The most striking finding was that having the wrong microbes in the wrong place reshaped the tissue identity to make it more suitable for them. DeLeon saw that mismatches changed gene and protein expression in the intestinal lining in ways that more closely resembled expression levels from the microbes’ original or native intestinal regions.
“It’s like they’re engineering or terraforming their environments to help them fit in,” DeLeon said.
An ‘omni-microbial’ approach
Chang said that this research highlights the need for more caution with FMT before we fully understand the long-term effects of introducing one set of microbes into a new environment.
“We have absolutely no idea what’s in FMT, except that it’s a combination of microbes,” Chang said.
“But even a single FMT will cause a change in the host-microbe relationships in these very different regions of the bowel that may be very difficult to reverse.”
Both DeLeon and Chang advocate for “omni-microbial transplants,” or OMT, instead. This approach would transfer microbes taken from all the different regions of the intestine, not just those largely from the colon.
“Whether given via an endoscopy or in pill form, microbes naturally settle in the right places, especially when they are competing side by side with others that normally inhabit a certain region.
“If there’s an open space, something’s going to fill it,” DeLeon said. “But the microbes that were supposed to be there are better suited for it, so they’re more naturally going to fill it even in the presence of other microbes.”
DeLeon plans to keep studying how different microbes exert their influence in different parts of the intestine, using different approaches like single cell sequencing and metabolomics to track their activity.
He is also exploring how the gut regions terraformed by microbiota mismatches can be restored to their original state, which could help restore normal gut function. Such deeper understanding could lead to improvements in the application of microbial transplants, ultimately helping them live up to their significant promise.
Funding: The study, “Regional microbiota mismatches from fecal microbiota transplants promote persistent, off-target consequences to the host,” was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases and the UChicago GI Research Foundation.
Additional authors include Mora Mocanu, Candace M. Cham, Alan Tan, Ashley M. Sidebottom, Jason Koval, Hugo D. Ceccato, John J. Colgan, Marissa M. St. George, Joash M. Lake, Michael Cooper, Jingwen Xu, and David T. Rubin from UChicago; Julia Moore and Kristina Martinez-Guryn from Midwestern University; and Zhilu Xu, Siew C. Ng, Francis K.L. Chan, Hein M. Tun, and Qi Su from the Chinese University of Hong Kong.
About this neuroscience research news
Author: Orlando DeLeon
Source: University of Chicago
Contact: Orlando DeLeon – University of Chicago
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Microbiome mismatches from microbiota transplants lead to persistent off-target metabolic and immunomodulatory effects” by Orlando DeLeon et al. Cell
Abstract
Microbiome mismatches from microbiota transplants lead to persistent off-target metabolic and immunomodulatory effects
Fecal microbiota transplant (FMT) is an increasingly used intervention, but its suitability to restore regional gut microbiota, particularly in the small bowel (SB), must be questioned because of its predominant anaerobic composition.
In human subjects receiving FMT by upper endoscopy, duodenal engraftment of anaerobes was observed after 4 weeks. We hypothesized that peroral FMTs create host-microbe mismatches that impact SB homeostasis.
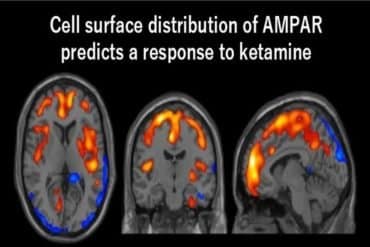
To test this, antibiotic-treated specific-pathogen-free (SPF) mice were given jejunal, cecal, or fecal microbiota transplants (JMTs, CMTs, or FMTs, respectively) and studied 1 or 3 months later.
JMT and FMT altered regional microbiota membership and function, energy balance, and intestinal and hepatic transcriptomes; JMT favored host metabolic pathways and FMT favored immune pathways.
MTs drove regional intestinal identity (Gata4, Gata6, and Satb2) and downstream differentiation markers. RNA sequencing (RNA-seq) of metabolite-exposed human enteroids and duodenal biopsies post-FMT confirmed transcriptional changes in mice.
Thus, regional microbial mismatches after FMTs can lead to unintended consequences and require rethinking of microbiome-based interventions.