Summary: Researchers have identified a specific brain circuit that allows voluntary control of breathing, linking it to emotional and behavioral states. This circuit, spanning the anterior cingulate cortex, pons, and medulla, slows breathing during calm states and accelerates it under anxiety. Experiments in mice showed activating this circuit reduced anxiety, while shutting it off increased stress.
The findings provide a neurological basis for practices like yoga and mindfulness and suggest potential therapeutic targets for anxiety and panic disorders. Scientists aim to develop drugs that could stimulate this circuit to regulate breathing and alleviate stress. This discovery highlights how breathing can influence mental well-being through direct brain mechanisms.
Key Facts:
- A brain circuit connecting the cortex, pons, and medulla coordinates breathing with emotions.
- Activating the circuit slowed breathing and reduced anxiety in mice.
- Findings could inspire drugs to regulate breathing and treat anxiety disorders.
Source: Salk Institute
Deep breath in, slow breath out…
Isn’t it odd that we can self-soothe by slowing down our breathing?
Humans have long used slow breathing to regulate their emotions, and practices like yoga and mindfulness have even popularized formal techniques like box breathing. Still, there has been little scientific understanding of how the brain consciously controls our breathing and whether this actually has a direct effect on our anxiety and emotional state.
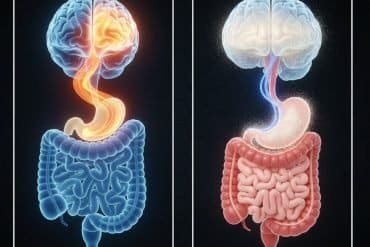
Neuroscientists at the Salk Institute have now, for the first time, identified a specific brain circuit that regulates breathing voluntarily. Using mice, the researchers pinpointed a group of brain cells in the frontal cortex that connects to the brainstem, where vital actions like breathing are controlled.
Their findings suggest this connection between the more sophisticated parts of the brain and the lower brainstem’s breathing center allows us to coordinate our breathing with our current behaviors and emotional state.
The findings, published in Nature Neuroscience on November 19, 2024, describe a new set of brain cells and molecules that could be targeted with therapeutics to prevent hyperventilation and regulate anxiety, panic, or post-traumatic stress disorders.
“The body naturally regulates itself with deep breaths, so aligning our breathing with our emotions seems almost intuitive to us—but we didn’t really know how this worked in the brain,” says senior author Sung Han, associate professor and Pioneer Fund Developmental Chair at Salk.
“By uncovering a specific brain mechanism responsible for slowing breathing, our discovery may offer a scientific explanation for the beneficial effects of practices like yoga and mindfulness on alleviating negative emotions, grounding them further in science.”
Breathing patterns and emotional state are difficult to untangle—if anxiety increases or decreases, so does the breathing rate. Despite this seemingly obvious connection between emotional regulation and breathing, previous studies had only thoroughly explored subconscious breathing mechanisms in the brainstem.
And while newer studies had started to describe conscious top-down mechanisms, no specific brain circuits were discovered until the Salk team took a crack at the case.
The researchers assumed the brain’s frontal cortex, which orchestrates complex thoughts and behaviors, was somehow communicating to a brainstem region called the medulla, which controls automatic breathing.
To test this, they first consulted a neural connectivity database and then did experiments to trace the connections between these different brain areas.
These initial experiments revealed a potential new breathing circuit: Neurons in a frontal region called the anterior cingulate cortex were connected to an intermediate brainstem area in the pons, which was then connected to the medulla just below.
Beyond the physical connections of these brain areas, it was also important to consider the types of messages they might send each other. For example, when the medulla is active, it initiates breathing.
However, messages coming down from the pons actually inhibit activity in the medulla, leading breathing rates to slow down. Han’s team hypothesized that certain emotions or behaviors could lead cortical neurons to activate the pons, which would then lower activity in the medulla, resulting in slower breath.
To test this, the researchers recorded brain activity in mice during behaviors that alter breathing, such as sniffing, swimming, and drinking, as well as during conditions that induce fear and anxiety.
They also used a technique called optogenetics to turn parts of this brain circuit on or off in different emotional and behavioral contexts while measuring the animals’ breathing and behavior.
Their findings confirmed that when the connection between the cortex and the pons was activated, mice were calmer and breathed more slowly, but when mice were in anxiety-inducing situations, this communication decreased, and breathing rates went up.
Furthermore, when the researchers artificially activated this cortex-pons-medulla circuit, the animals’ breath slowed, and they showed fewer signs of anxiety. On the other hand, if researchers shut this circuit off, breathing rates went up, and the mice became more anxious.
Altogether, this anterior cingulate cortex-pons-medulla circuit supported the voluntary coordination of breathing rates with behavioral and emotional states.
“Our findings got me thinking: Could we develop drugs to activate these neurons and manually slow our breathing or prevent hyperventilation in panic disorder?” says first author of the study Jinho Jhang, a senior research associate in Han’s lab.
“My sister, three years younger than me, has suffered from panic disorder for many years. She continues to inspire my research questions and my dedication to answering them.”
The researchers will continue analyzing the circuit to determine whether drugs could activate it to slow breathing on command. Additionally, the team is working to find the circuit’s converse—a fast breathing circuit, which they believe is likely also tied to emotion.
They are hopeful their findings will result in long-term solutions for people with anxiety, stress, and panic disorders, who inspire their discovery and dedication.
“I want to use these findings to design a yoga pill,” says Han.
“It may sound silly, and the translation of our work into a marketable drug will take years, but we now have a potentially targetable brain circuit for creating therapeutics that could instantly slow breathing and initiate a peaceful, meditative state.”
Other authors include Shijia Liu, Seahyung Park, and David O’Keefe of Salk.
Funding: The work was supported by the Kavli Institute for Brain and Mind (IRGS 2020-1710).
About this emotion and breathing research news
Author: Salk Comm
Source: Salk Institute
Contact: Salk Comm – Salk Institute
Image: The image is credited to Neuroscience News
Original Research: Closed access.
“A top-down slow breathing circuit that alleviates negative affect” by Sung Han et al. Nature Neuroscience
Abstract
A top-down slow breathing circuit that alleviates negative affect
Although breathing is primarily automatic, its modulation by behavior and emotions suggests cortical inputs to brainstem respiratory networks, which hitherto have received little characterization.
Here we identify in mice a top-down breathing pathway from dorsal anterior cingulate cortex (dACC) neurons to pontine reticular nucleus GABAergic inhibitory neurons (PnCGABA), which then project to the ventrolateral medulla (VLM).
dACC→PnC activity correlates with slow breathing cycles and volitional orofacial behaviors and is influenced by anxiogenic conditions.
Optogenetic stimulation of the dACC→PnCGABA→VLM circuit simultaneously slows breathing and suppresses anxiety-like behaviors, whereas optogenetic inhibition increases both breathing rate and anxiety-like behaviors.
These findings suggest that the dACC→PnCGABA→VLM circuit has a crucial role in coordinating slow breathing and reducing negative affect. Our study elucidates a circuit basis for top-down control of breathing, which can influence emotional states.