Summary: A new stem cell therapy approach eliminates established brain tumors and provides long-term immunity, training the immune system to prevent cancer from returning.
Source: Brigham and Women’s Hospital
Scientists are harnessing a new way to turn cancer cells into potent, anti-cancer agents.
In the latest work from the lab of Khalid Shah, MS, Ph.D., at Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, investigators have developed a new cell therapy approach to eliminate established tumors and induce long-term immunity, training the immune system so that it can prevent cancer from recurring.
The team tested their dual-action, cancer-killing vaccine in an advanced mouse model of the deadly brain cancer glioblastoma, with promising results.
Findings are published in Science Translational Medicine.
“Our team has pursued a simple idea: to take cancer cells and transform them into cancer killers and vaccines,” said corresponding author Khalid Shah, MS, Ph.D., director of the Center for Stem Cell and Translational Immunotherapy (CSTI) and the vice chair of research in the Department of Neurosurgery at the Brigham and faculty at Harvard Medical School and Harvard Stem Cell Institute (HSCI).
“Using gene engineering, we are repurposing cancer cells to develop a therapeutic that kills tumor cells and stimulates the immune system to both destroy primary tumors and prevent cancer.”
Cancer vaccines are an active area of research for many labs, but the approach that Shah and his colleagues have taken is distinct. Instead of using inactivated tumor cells, the team repurposes living tumor cells, which possess an unusual feature. Like homing pigeons returning to roost, living tumor cells will travel long distances across the brain to return to the site of their fellow tumor cells.
Taking advantage of this unique property, Shah’s team engineered living tumor cells using the gene editing tool CRISPR-Cas9 and repurposed them to release tumor cell killing agent.
In addition, the engineered tumor cells were designed to express factors that would make them easy for the immune system to spot, tag and remember, priming the immune system for a long-term anti-tumor response.
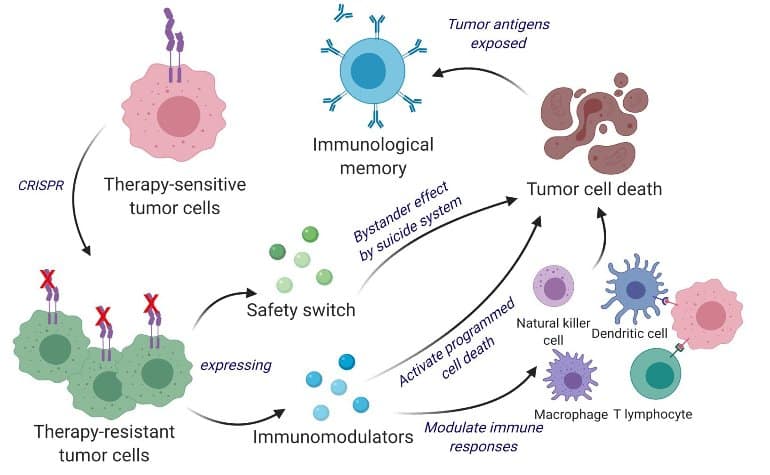
The team tested their repurposed CRISPR-enhanced and reverse-engineered therapeutic tumor cells (ThTC) in different mice strains including the one that bore bone marrow, liver and thymus cells derived from humans, mimicking the human immune microenvironment. Shah’s team also built a two-layered safety switch into the cancer cell, which, when activated, eradicates ThTCs if needed.
This dual-action cell therapy was safe, applicable, and efficacious in these models, suggesting a roadmap toward therapy. While further testing and development is needed, Shah’s team specifically chose this model and used human cells to smooth the path of translating their findings for patient settings.
“Throughout all of the work that we do in the Center, even when it is highly technical, we never lose sight of the patient,” said Shah.
“Our goal is to take an innovative but translatable approach so that we can develop a therapeutic, cancer-killing vaccine that ultimately will have a lasting impact in medicine.”
Shah and colleagues note that this therapeutic strategy is applicable to a wider range of solid tumors and that further investigations of its applications are warranted.
About this brain cancer research news
Author: Press Office
Source: Brigham and Women’s Hospital
Contact: Press Office – Brigham and Women’s Hospital
Image: The image is credited to Kok Siong Chen and Khalid Shah
Original Research: Open access.
“Bifunctional cancer cell-based vaccine concomitantly drives direct tumor killing and antitumor immunity” by Kok-Siong Chen et al. Science Translational Medicine
Abstract
Bifunctional cancer cell-based vaccine concomitantly drives direct tumor killing and antitumor immunity
The administration of inactivated tumor cells is known to induce a potent antitumor immune response; however, the efficacy of such an approach is limited by its inability to kill tumor cells before inducing the immune responses. Unlike inactivated tumor cells, living tumor cells have the ability to track and target tumors.
Here, we developed a bifunctional whole cancer cell–based therapeutic with direct tumor killing and immunostimulatory roles. We repurposed the tumor cells from interferon-β (IFN-β) sensitive to resistant using CRISPR-Cas9 by knocking out the IFN-β–specific receptor and subsequently engineered them to release immunomodulatory agents IFN-β and granulocyte-macrophage colony-stimulating factor.
These engineered therapeutic tumor cells (ThTCs) eliminated established glioblastoma tumors in mice by inducing caspase-mediated cancer cell apoptosis, down-regulating cancer-associated fibroblast-expressed platelet-derived growth factor receptor β, and activating antitumor immune cell trafficking and antigen-specific T cell activation signaling.
This mechanism-based efficacy of ThTCs translated into a survival benefit and long-term immunity in primary, recurrent, and metastatic cancer models in immunocompetent and humanized mice. The incorporation of a double kill-switch comprising herpes simplex virus–1 thymidine kinase and rapamycin-activated caspase 9 in ThTCs ensured the safety of our approach.
Arming naturally neoantigen-rich tumor cells with bifunctional therapeutics represents a promising cell-based immunotherapy for solid tumors and establishes a road map toward clinical translation.







