Summary: A new study reveals that increasing levels of apolipoprotein M (ApoM) may slow or prevent the progression of age-related macular degeneration (AMD), a major cause of blindness in older adults. Researchers found that low ApoM impairs cholesterol metabolism in the retina, contributing to inflammation and vision loss—especially in advanced forms like geographic atrophy.
In mouse models, boosting ApoM improved retinal health and reduced cholesterol buildup by activating a protective signaling pathway with sphingosine-1-phosphate (S1P). The findings suggest a potential therapy that could not only preserve vision but also benefit patients with heart failure, which shares similar cholesterol-processing dysfunction.
Key Facts:
- ApoM Deficiency: Low ApoM disrupts cholesterol metabolism in the eye and heart, triggering inflammation and cell damage.
- Therapeutic Potential: Raising ApoM levels improved retinal health and reduced lipid buildup in mouse models of AMD.
- Dual Benefit: Findings may lead to new treatments for both macular degeneration and heart failure.
Source: WUSTL
A new study from Washington University School of Medicine in St. Louis identifies a possible way to slow or block progression of age-related macular degeneration, a leading cause of blindness in people over age 50.
The WashU Medicine researchers and their international collaborators implicated problems with cholesterol metabolism in this type of vision loss, perhaps helping to explain the links between macular degeneration and cardiovascular disease, which both worsen with age.
The new findings — identified using human plasma samples and mouse models of macular degeneration — suggest that increasing the amount of a molecule called apolipoprotein M (ApoM) in the blood fixes problems in cholesterol processing that lead to cellular damage in the eyes and other organs.
Various methods of dialing up ApoM could serve as new treatment strategies for age-related macular degeneration and perhaps some forms of heart failure triggered by similar dysfunctional cholesterol processing.
The study appears June 24 in the journal Nature Communications.
“Our study points to a possible way to address a major unmet clinical need,” said senior author Rajendra S. Apte, MD, PhD, the Paul A. Cibis Distinguished Professor of Ophthalmology and Visual Sciences at WashU Medicine.
“Current therapies that reduce the chance of further vision loss are limited to only the most advanced stages of macular degeneration and do not reverse the disease. Our findings suggest that developing treatments that increase ApoM levels could treat or even prevent the disease and therefore preserve people’s vision as they age.”
In macular degeneration, doctors can see cholesterol-rich deposits under the retina during an eye exam, according to Apte. In early stages, vision might still be normal, but the deposits increase inflammation and other damaging processes the lead to the gradual loss of central vision.
In the most common type, “dry” macular degeneration, the cells in the central part of the retina can be damaged, causing a type of neurodegeneration called geographic atrophy, which is similar to what happens in the brain in conditions such as Alzheimer’s disease. Dry macular degeneration can turn into “wet” macular degeneration, in which abnormal blood vessel growth damages vision.
Geographic atrophy and wet macular degeneration are advanced forms of the disease that are accompanied by vision loss. Although some approved therapies for advanced disease are available, the disease process itself is not reversible at that stage.
A common culprit in eye disease and heart failure
In recent years, evidence has emerged that ApoM can serve as a protective molecule with known anti-inflammatory effects and roles in maintaining healthy cholesterol metabolism.
With that in mind, Apte and co-senior author Ali Javaheri, MD, PhD, an assistant professor of medicine, were interested assessing whether reduced ApoM levels, which fall with age, could be involved in the dysfunctional cholesterol metabolism that is at the root of multiple diseases of aging, including macular degeneration and heart disease.
They showed that patients with macular degeneration have reduced levels of ApoM circulating in the blood compared with healthy controls. And past work by Javaheri, a WashU Medicine cardiologist, showed that patients with various forms of heart failure also had reduced levels of ApoM in the blood.
This study revealed that ApoM is a key component in the “good cholesterol” pathways that mop up excess cholesterol — the bad kind that tends to drive inflammation — and clear it from the body through the liver.
Apte and Javaheri’s research suggests that when ApoM is low, cells in the retina and heart muscle can’t correctly metabolize cholesterol deposits and have a hard time getting rid of these accumulating lipids. When these lipids build up, it leads to inflammation and cellular damage.
To see if they could reverse the harmful effects of low ApoM, the researchers increased ApoM levels in mouse models of macular degeneration, using genetic modification or plasma transfer from other mice.
The mice showed evidence of improved retinal health, improved function of light-sensing cells in the retina and reduced accumulation of cholesterol deposits.
The researchers further found evidence that ApoM triggers a signaling pathway that breaks down the cholesterol in cellular compartments called lysosomes, which are known for playing important roles in disposing of cellular waste.
The researchers also found that ApoM must be bound to a molecule called sphingosine-1-phosphate (S1P) to get the beneficial effects of ApoM treatment in the mice.
Apte and Javaheri are working with Mobius Scientific, a WashU startup company that is working to harness this knowledge of the role of ApoM in macular degeneration to develop new approaches to treating or preventing the disease. Apte and Javaheri worked with WashU’s Office of Technology Management (OTM) to launch Mobius Scientific in 2022.
The findings also could have implications for future interventions that raise ApoM in patients with heart failure.
“One of the exciting things about this collaboration is realizing the links between retinal pigment epithelial cells and heart muscle cell, which are both vulnerable to low ApoM,” Javeheri said.
“It is possible that the interaction between ApoM and S1P is regulating cholesterol metabolism in both cell types. We look forward to exploring strategies to increase ApoM in ways that could help the eye and the heart maintain healthy cholesterol metabolism over time and stave off two major diseases of aging.”
Funding: This work was supported by National Institutes of Health (NIH), grant numbers R01 EY019287, P30 EY02687, 1T32GM1397740-1, K08HL138262, 1R01HL155344, P30DK020579 and P30DK056341; the Jeffrey T. Fort Innovation Fund; the Starr Foundation AMD Research Fund; the Siteman Retina Research Fund; a Research to Prevent Blindness/American Macular Degeneration Foundation Catalyst Award for Innovative Research Approaches for Age-Related Macular Degeneration; the Carl Marshall and Mildred Almen Reeves Foundation; the Retina Associates of St. Louis Research Fund; a pilot project grant from the Washington University Genome Technology Access Center; an unrestricted grant from Research to Prevent Blindness to the John F. Hardesty, MD Department of Ophthalmology and Visual Sciences at Washington University School of Medicine in St. Louis; a Vitreoretinal Surgery Foundation Fellowship, number VGR0023118; the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital, grant number MC-FR-2020- 919; the Longer Life Foundation; and by the Austrian Science Fund, grant number SFB 10.55776/F73.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Apte and Javaheri have intellectual property applications licensed by Washington University to Mobius Scientific. Apte is currently the chief scientific officer at Mobius Scientific and both serve on the company’s advisory board.
About this AMD and genetics research news
Author: Abeeha Shamshad
Source: WUSTL
Contact: Abeeha Shamshad – WUSTL
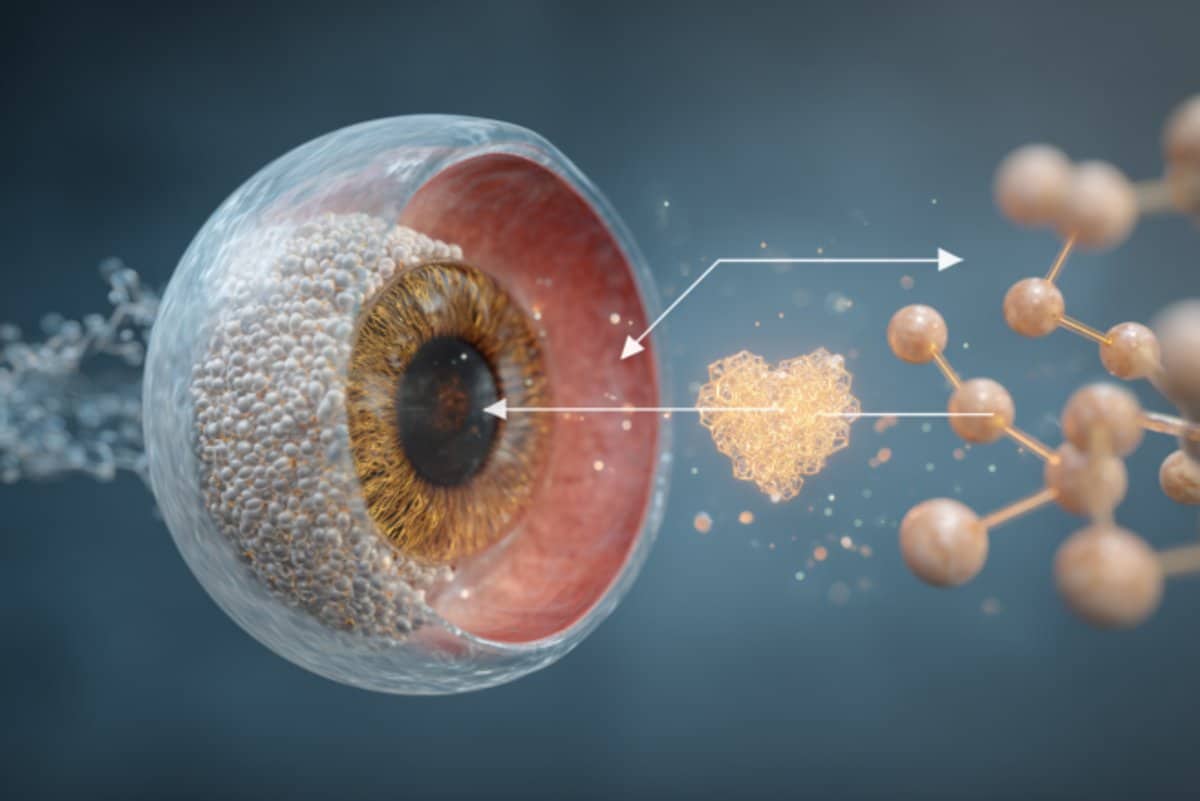
Image: The image is credited to Neuroscience News
Original Research: Open access.
“Apolipoprotein M attenuates age-related macular degeneration phenotypes via sphingosine-1-phosphate signaling and lysosomal lipid catabolism” by Rajendra S. Apte et al. Nature Communications
Abstract
Apolipoprotein M attenuates age-related macular degeneration phenotypes via sphingosine-1-phosphate signaling and lysosomal lipid catabolism
Age-related macular degeneration (AMD) is a leading cause of blindness in people over 50. AMD and cardiovascular disease share risk factors including age, impaired lipid metabolism, and extracellular lipid deposition.
Because of its importance in age-related diseases, we hypothesize that apolipoprotein M (ApoM), a lipocalin that binds sphingosine-1-phosphate (S1P), might restore lipid homeostasis and retinal function in AMD.
In support, we find that human patients with AMD demonstrate significantly reduced ApoM compared to controls.
In mice with impaired retinal cholesterol efflux, ApoM improves retinal pigment epithelium (RPE) function and lipotoxicity in an S1P- and S1P receptor 3-dependent manner.
Ultrastructural evidence of enhanced melanosome-lipid droplet interactions led us to hypothesize and demonstrate that ApoM-S1P signaling drives RPE-specific lysosomal lipid catabolism. RPE-specific knockout of lysosomal acid lipase recapitulates features of AMD.
Our study defines a novel role for ApoM/S1P signaling in AMD driven by RPE lipotoxicity, mediated by cell-autonomous lysosomal lipid catabolism.







