Summary: A new study paves the way for potential treatments for Multiple Sclerosis (MS) by identifying the OTC antihistamine, clemastine, as an effective drug for brain repair. Utilizing a newly-developed MRI scan technique, scientists were able to observe and measure the impact of clemastine on brain myelin levels.
The study offers the first documented example of brain repair for a chronic neurological condition through MRI. These results are expected to set a standard for future research into myelin-rebuilding therapies.
Key Facts:
- Clemastine, an over-the-counter antihistamine, has been identified as a potential therapy for MS, with observed increases in myelin water fraction indicating myelin repair.
- A unique MRI technique was used to measure changes in myelin levels before and after the drug was administered, setting a new standard for tracking myelin recovery.
- Beyond its potential impact on MS, clemastine is also being considered for use in treating brain injury in premature infants, who often experience myelin damage.
Source: UCSF
A decade after UC San Francisco scientists identified an over-the-counter antihistamine as a treatment for multiple sclerosis, researchers have developed an approach to measure the drug’s effectiveness in repairing the brain, making it possible to also assess future therapies for the devastating disorder.
The researchers, led by physician-scientist Ari Green, MD, who together with neuroscientist Jonah Chan, Ph.D., first identified clemastine as a potential MS therapy, used MRI scans to study the drug’s impact on the brain of 50 participants in a clinical study.
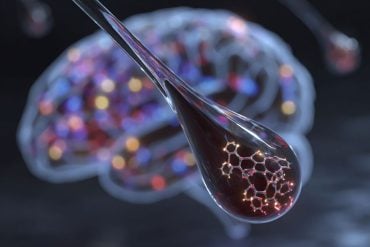
In MS, patients lose myelin, the protective insulation around nerve fibers. This myelin loss triggers delays in nerve signals, leading to weakness and spasticity, vision loss, cognitive slowing and other symptoms.

In the brain, water trapped between the thin layers of myelin that wrap nerve fibers cannot move as freely as water floating between brain cells.
This unique property of myelin allowed imaging experts to develop a technique to compare the difference in myelin levels before and after the drug was administered, by measuring the so-called myelin water fraction, or the ratio of myelin water to the total water content in brain tissue.
In their study, published May 8, 2023, in PNAS, the researchers found that patients with MS who were treated with clemastine experienced modest increases in myelin water, indicating myelin repair.
They also proved that the myelin water fraction technique, when focused on the right parts of the brain, could be used to track myelin recovery.
“This is the first example of brain repair being documented on MRI for a chronic neurological condition,” said Green, medical director of the UCSF Multiple Sclerosis and Neuroinflammation Center and a member of the Weill Institute for Neurosciences.
“The study provides the first direct, biologically validated, imaging-based evidence of myelin repair induced by clemastine. This will set the standard for future research into remyelinating therapies.”
Myelin increased even after medication was stopped
In the study, patients with MS who enrolled in the ReBUILD trial were divided into two groups: the first group received clemastine for the first three months of the study and the second group received clemastine only in months three to five.
Using the myelin water fraction as a biomarker, the researchers found that myelin water increased in the first group after participants received the drug and continued to increase after clemastine was stopped.
In the second group, the myelin water fraction showed decreases in myelin water in the first portion of the study, under the placebo, and a rebound after participants received clemastine.
The findings corroborate the results of a previous study with the same 50 patients that had found the allergy medication reduced delayed nerve signaling, potentially alleviating symptoms.
In the current study, researchers looked at the corpus callosum, a region of the brain with a high myelin content that connects the right and left hemispheres.
They found that significant repair occurred outside the visible lesions typically associated with MS. This underscores the need to focus on myelin repair beyond these lesion sites.
Clemastine works in this setting by stimulating the differentiation of myelin-making stem cells. This places the medication a generation ahead of existing MS drugs that work by dampening the activity of the immune system, calming inflammation and reducing the risk of relapse. It still isn’t ideal, though, making the water fraction measurement an important tool in developing better therapeutics.
“Clemastine can only be partially effective at the doses we can use,” said Green, who is also a neuro-ophthalmologist and chief of the Division of Neuroimmunology and Glial Biology in the UCSF Department of Neurology.
“It can be sedating, which may be especially undesirable in patients with MS. We are hopeful better medications will be developed, but clemastine has proven to be the tool to show remyelination is possible.”
Proposed future research will examine clemastine’s potential in treating brain injury in premature infants, who often experience myelin damage.
Pediatric neurologist Bridget Ostrem, MD, Ph.D., of UCSF Benioff Children’s Hospitals, is currently seeking approval from the Food and Drug Administration to initiate the first clinical trial testing clemastine to treat this debilitating and disabling condition.
About this neuropharmacology and Multiple Sclerosis research news
Author: Ari Green
Source: UCSF
Contact: Ari Green – UCSF
Image: The image is credited to Neuroscience News
Original Research: Open access.
“MWF of the corpus callosum is a robust measure of remyelination: Results from the ReBUILD trial” by Ari Green et al. PNAS
Abstract
MWF of the corpus callosum is a robust measure of remyelination: Results from the ReBUILD trial
Myelin repair is an unrealized therapeutic goal in the treatment of multiple sclerosis (MS). Uncertainty remains about the optimal techniques for assessing therapeutic efficacy and imaging biomarkers are required to measure and corroborate myelin restoration.
We analyzed myelin water fraction imaging from ReBUILD, a double-blind, randomized placebo-controlled (delayed treatment) remyelination trial, that showed a significant reduction in VEP latency in patients with MS.
We focused on brain regions rich in myelin. Fifty MS subjects in two arms underwent 3T MRI at baseline and months 3 and 5.
Half of the cohort was randomly assigned to receive treatment from baseline through 3 mo, whereas the other half received treatment from 3 mo to 5 mo post-baseline. We computed myelin water fraction changes occurring in normal-appearing white matter of corpus callosum, optic radiations, and corticospinal tracts.
An increase in myelin water fraction was documented in the normal-appearing white matter of the corpus callosum, in correspondence with the administration of the remyelinating treatment clemastine.
This study provides direct, biologically validated imaging-based evidence of medically induced myelin repair. Moreover, our work strongly suggests that significant myelin repair occurs outside of lesions.
We therefore propose myelin water fraction within the normal-appearing white matter of the corpus callosum as a biomarker for clinical trials looking at remyelination.