Summary: Using AI technology to analyze CMR scans, researchers were able to precisely quantify the blood flow to the heart muscles of patients. Comparing the AI-generated blood flow results with health outcomes, the team found those with reduced blood flow were at increased risk of stroke, heart attacks, and heart failure. The machine-learning algorithm was able to predict which patients may die or suffer major adverse health events better than doctors could.
Source: UCL
Artificial intelligence has been used for the first time to instantly and accurately measure blood flow, in a study led by UCL and Barts Health NHS Trust.
The results were found to be able to predict chances of death, heart attack and stroke, and can be used by doctors to help recommend treatments which could improve a patient’s blood flow.
Heart disease is the leading global cause of death and illness. Reduced blood flow, which is often treatable, is a common symptom of many heart conditions. International guidelines therefore recommend a number of assessments to measure a patient’s blood flow, but many are invasive and carry a risk.
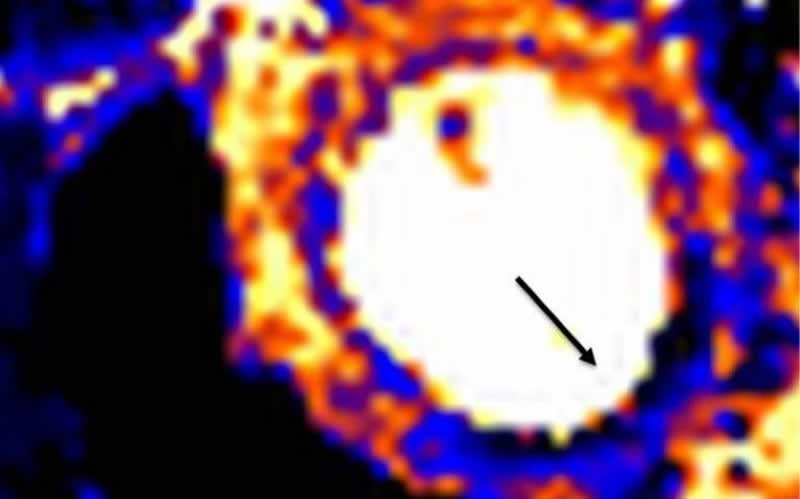
Non-invasive blood flow assessments are available, including Cardiovascular Magnetic Resonance (CMR) imaging, but up until now, the scan images have been incredibly difficult to analyse in a manner precise enough to deliver a prognosis or recommend treatment.
In the largest study of its kind, funded by British Heart Foundation and published in the journal Circulation, researchers took routine CMR scans from more than 1,000 patients attending St Bartholomew’s Hospital and the Royal Free Hospital and used a new automated artificial intelligence technique to analyse the images. By doing this, the teams were able to precisely and instantaneously quantify the blood flow to the heart muscle and deliver the measurements to the medical teams treating the patients.
By comparing the AI-generated blood flow results with the health outcomes of each patient, the team found that the patients with reduced blood flow were more likely to have adverse health outcomes including death, heart attack, stroke and heart failure.
The AI technique was therefore shown for the first time to be able to predict which patients might die or suffer major adverse events, better than a doctor could on their own with traditional approaches.
Professor James Moon (UCL Institute of Cardiovascular Science and Barts Health NHS Trust) said: “Artificial intelligence is moving out of the computer labs and into the real world of healthcare, carrying out some tasks better than doctors could do alone. We have tried to measure blood flow manually before, but it is tedious and time-consuming, taking doctors away from where they are needed most, with their patients.”
Dr Kristopher Knott (UCL Institute of Cardiovascular Science and Barts Health NHS Trust) added: “The predictive power and reliability of the AI was impressive and easy to implement within a patient’s routine care. The calculations were happening as the patients were being scanned, and the results were immediately delivered to doctors. As poor blood flow is treatable, these better predictions ultimately lead to better patient care, as well as giving us new insights into how the heart works.”
Dr Peter Kellman from the National Institutes of Health (NIH) in the US, who working with Dr Hui Xue at the NIH, developed the automated AI techniques to analyse the images that were used in the study, said: “This study demonstrates the growing potential of artificial intelligence-assisted imaging technology to improve the detection of heart disease and may move clinicians closer to a precision medicine approach to optimize patient care. We hope that this imaging approach can save lives in the future.”
Dr Kellman is director of the Medical Signal and Image Processing Program at the National Heart, Lung, and Blood Institute, part of the NIH.
Funding: The study was funded by the British Heart Foundation, National Institute for Health Research, European Regional Development Fund and Barts Charity, and involved additional researchers from the Royal Free Hospital, Queen Mary University of London and the University of Leeds.
Source:
UCL
Media Contacts:
Chris Lane – UCL
Image Source:
The image is credited to Kristopher Knott et al.
Original Research: Open access
“The Prognostic Significance of Quantitative Myocardial Perfusion: An Artificial Intelligence Based Approach Using Perfusion Mapping”. Kristopher D. Knott, Andreas Seraphim, Joao B. Augusto, Hui Xue, Liza Chacko, Nay Aung, Steffen E. Petersen, Jackie A. Cooper, Charlotte Manisty, Anish N. Bhuva, Tushar Kotecha, Christos V. Bourantas, Rhodri H. Davies, Louise A.E. Brown, Sven Plein, Marianna Fontana, Peter Kellman, and James C. Moon.
Circulation doi:10.1161/CIRCULATIONAHA.119.044666.
Abstract
The Prognostic Significance of Quantitative Myocardial Perfusion: An Artificial Intelligence Based Approach Using Perfusion Mapping
Background: Myocardial perfusion reflects the macro- and microvascular coronary circulation. Recent quantitation developments using cardiovascular magnetic resonance (CMR) perfusion permit automated measurement clinically. We explored the prognostic significance of stress myocardial blood flow (MBF) and myocardial perfusion reserve (MPR, the ratio of stress to rest MBF).
Methods: A two center study of patients with both suspected and known coronary artery disease referred clinically for perfusion assessment. Image analysis was performed automatically using a novel artificial intelligence approach deriving global and regional stress and rest MBF and MPR. Cox proportional hazard models adjusting for co-morbidities and CMR parameters sought associations of stress MBF and MPR with death and major adverse cardiovascular events (MACE), including myocardial infarction, stroke, heart failure hospitalization, late (>90 day) revascularization and death.
Results: 1049 patients were included with median follow-up 605 (interquartile range 464-814) days. There were 42 (4.0%) deaths and 188 MACE in 174 (16.6%) patients. Stress MBF and MPR were independently associated with both death and MACE. For each 1ml/g/min decrease in stress MBF the adjusted hazard ratio (HR) for death and MACE were 1.93 (95% CI 1.08-3.48, P=0.028) and 2.14 (95% CI 1.58-2.90, P<0.0001) respectively, even after adjusting for age and co-morbidity. For each 1 unit decrease in MPR the adjusted HR for death and MACE were 2.45 (95% CI 1.42-4.24, P=0.001) and 1.74 (95% CI 1.36-2.22, P<0.0001) respectively. In patients without regional perfusion defects on clinical read and no known macrovascular coronary artery disease (n=783), MPR remained independently associated with death and MACE, with stress MBF remaining associated with MACE only.
Conclusions: In patients with known or suspected coronary artery disease, reduced MBF and MPR measured automatically inline using artificial intelligence quantification of CMR perfusion mapping provides a strong, independent predictor of adverse cardiovascular outcomes.






