Summary: Researchers have discovered a unique pattern of scarring in the brains of those who were exposed to blast brain injuries that differs from those exposed to other types of head injury.
Source: USU.
Study identifies biological changes in the brain due to blast related TBI.
Scientists have discovered a unique pattern of scarring in the brains of deceased service members who were exposed to blast injury that differs from those exposed to other types of head injury. This new research was published online June 9 in Lancet Neurology, “Characterisation of Interface Astroglial Scarring in the Human Brain after Blast Exposure: a Post-mortem Case Series.”
“Our findings revealed those with blast exposure showed a distinct and previously unseen pattern of scarring, which involved the portion of brain tissue immediately beneath the superficial lining of the cerebral cortex – the junction between the gray and white matter – and the vital structures that are adjacent to the cavities within the brain that are filled with cerebrospinal fluid. Those areas of the brain, damaged by blast, suggest that they may be correlated with the symptoms displayed by those who sustained a traumatic brain injury, or TBI,” said Dr. Daniel Perl, study senior author and professor of Neuropathology at the Uniformed Services University of the Health Sciences. “This scarring pattern also suggests the brain has attempted to repair brain damage from a blast injury.”
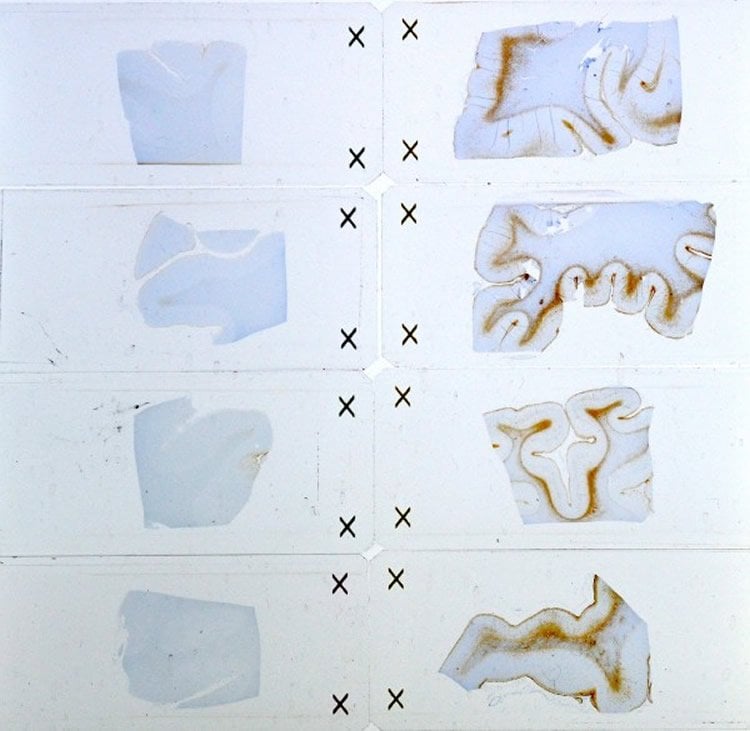
To better understand these blast brain injuries, researchers from the Uniformed Services University of the Health Sciences (USU), the Department of Defense Joint Pathology Center and the University of Colorado’s School of Medicine, examined brain tissue specimens derived from deceased service members, who had been exposed to a high explosive blast injury and had suffered several persistent symptoms. The researchers examined the brain tissues from five service members with remote blast exposures, as well as brain tissues of three service members who died shortly after severe blast exposures. They also compared these results with brain tissues from civilian (non-military) cases, including five with remote impact TBIs, and three cases with no history of a TBI.
“This changes the earlier paradigm of ‘battle injury’ and demonstrates unique and specific biological changes in brains due to these injuries,” said Perl, who also serves as director of USU’s Center for Neuroscience and Regenerative Medicine TBI Brain Tissue Repository.
Military members sustaining a TBI have often reported suffering from persistent post-concussive symptoms, which include a mixture of both neurologic and behavioral disturbances.
“These can include problems such as headaches, difficulty concentrating, sleep disorders, memory problems, depression and anxiety. Despite these prominent symptoms, conventional neuroimaging for mild TBIs typically has not allowed providers to “see” brain abnormalities, leading this to be considered the “invisible wound,” said Perl.
“This publication sheds some light, for the first time, into the nature of the persistent behavioral/ neurologic issues being reported in numerous service members who have been exposed to high explosives. It will certainly stimulate important further research and change how we think about these problems. DoD, through the Military Health System, is at the cutting edge of research dedicated to caring for our troops, and I hope that these findings will point the way into devising more rational approaches to their diagnosis, prevention and treatment,” Perl said.
Other members of the research team include co-lead authors Sharon Shively, MD, research assistant professor in USU’s Department of Pathology and USU contract employee of the Henry M. Jackson Foundation for the Advancement of Military Medicine; Iren Horkayne-Szakaly, M.D., neuropathologist and neuromuscular pathologist, Joint Pathology Center, Defense Health Agency; Robert V. Jones, M.D., senior neuropathologist, Joint Pathology Center, Defense Health Agency; James P. Kelly, M.D., professor of Neurosurgery and Physical Medicine & Rehabilitation, Colorado School of Medicine; and Regina C. Armstrong, M.D., professor of Anatomy, Physiology and Genetics, and director of USU’s Center for Neuroscience and Regenerative Medicine at USU.
Funding: Funding for the study was provided by the Defense Health Program.
Source: Sarah Marshall – USU
Image Source: This NeuroscienceNews.com image is credited to Uniformed Services University of the Health Sciences.
Original Research: Abstract for “Characterisation of interface astroglial scarring in the human brain after blast exposure: a post-mortem case series” by Sharon Baughman Shively, Iren Horkayne-Szakaly, Robert V Jones, James P Kelly, Regina C Armstrong, and Daniel P Perl in The Lancet. Published online June 9 2016 doi:10.1016/S1474-4422(16)30057-6
[cbtabs][cbtab title=”MLA”]USU. “Invisible Wounds of War Now Able to be Seen.” NeuroscienceNews. NeuroscienceNews, 10 June 2016.
<https://neurosciencenews.com/blast-tbi-neurology-4435/>.[/cbtab][cbtab title=”APA”]USU. (2016, June 10). Invisible Wounds of War Now Able to be Seen. NeuroscienceNews. Retrieved June 10, 2016 from https://neurosciencenews.com/blast-tbi-neurology-4435/[/cbtab][cbtab title=”Chicago”]USU. “Invisible Wounds of War Now Able to be Seen.” https://neurosciencenews.com/blast-tbi-neurology-4435/ (accessed June 10, 2016).[/cbtab][/cbtabs]
Abstract
Characterisation of interface astroglial scarring in the human brain after blast exposure: a post-mortem case series
Background
No evidence-based guidelines are available for the definitive diagnosis or directed treatment of most blast-associated traumatic brain injuries, partly because the underlying pathology is unknown. Moreover, few neuropathological studies have addressed whether blast exposure produces unique lesions in the human brain, and if those lesions are comparable with impact-induced traumatic brain injury. We aimed to test the hypothesis that blast exposure produces unique patterns of damage, differing from that associated with impact-induced, non-blast traumatic brain injuries.
Methods
In this post-mortem case series, we investigated several features of traumatic brain injuries, using clinical histopathology techniques and markers, in brain specimens from male military service members with chronic blast exposures and from those who had died shortly after severe blast exposures. We then compared these results with those from brain specimens from male civilian (ie, non-military) cases with no history of blast exposure, including cases with and without chronic impact traumatic brain injuries and cases with chronic exposure to opiates, and analysed the limited associated clinical histories of all cases. Brain specimens had been archived in tissue banks in the USA.
Findings
We analysed brain specimens from five cases with chronic blast exposure, three cases with acute blast exposure, five cases with chronic impact traumatic brain injury, five cases with exposure to opiates, and three control cases with no known neurological disorders. All five cases with chronic blast exposure showed prominent astroglial scarring that involved the subpial glial plate, penetrating cortical blood vessels, grey–white matter junctions, and structures lining the ventricles; all cases of acute blast exposure showed early astroglial scarring in the same brain regions. All cases of chronic blast exposure had an antemortem diagnosis of post traumatic stress disorder. The civilian cases, with or without history of impact traumatic brain injury or a history of opiate use, did not have any astroglial scarring in the brain regions analysed.
Interpretation
The blast exposure cases showed a distinct and previously undescribed pattern of interface astroglial scarring at boundaries between brain parenchyma and fluids, and at junctions between grey and white matter. This distinctive pattern of scarring may indicate specific areas of damage from blast exposure consistent with the general principles of blast biophysics, and further, could account for aspects of the neuropsychiatric clinical sequelae reported. The generalisability of these findings needs to be explored in future studies, as the number of cases, clinical data, and tissue availability were limited.
Funding
Defense Health Program of the United States Department of Defense.
“Characterisation of interface astroglial scarring in the human brain after blast exposure: a post-mortem case series” by Sharon Baughman Shively, Iren Horkayne-Szakaly, Robert V Jones, James P Kelly, Regina C Armstrong, and Daniel P Perl in The Lancet. Published online June 9 2016 doi:10.1016/S1474-4422(16)30057-6






