Summary: Brain aging is accelerated by up to 26% in those with progressive type 2 diabetes.
Source: Life
Scientists have demonstrated that normal brain aging is accelerated by approximately 26% in people with progressive type 2 diabetes compared to individuals without the disease, reports a study published today in Life.
The authors evaluated the relationship between typical brain aging and that seen in type 2 diabetes, and observed that type 2 diabetes follows a similar pattern of neurodegeneration as aging, but one that progresses faster.
One important implication of this finding is that even typical brain aging may reflect changes in the brain’s regulation of glucose by insulin.
The results further suggest that by the time type 2 diabetes is formally diagnosed, there may already be significant structural damage to the brain. Sensitive ways to detect diabetes-associated changes to the brain are therefore urgently needed.
There is already strong evidence linking type 2 diabetes with cognitive decline, yet few patients currently undergo a comprehensive cognitive assessment as part of their clinical care. It can be difficult to distinguish between normal brain aging that begins in middle age, and brain aging caused or accelerated by diabetes.
To date, no studies have directly compared neurological changes in healthy people over the course of their lifespan with changes to those experienced by people of the same age with diabetes.
“Routine clinical assessments for diagnosing diabetes typically focus on blood glucose, insulin levels and body mass percentage,” says first author Botond Antal, a Ph.D. student at the Department of Biomedical Engineering, Stony Brook University, New York, US.
“However, the neurological effects of type 2 diabetes may reveal themselves many years before they can be detected by standard measures, so by the time type 2 diabetes is diagnosed by conventional tests, patients may have already sustained irreversible brain damage.”
To define the impact of diabetes on the brain over and above normal aging, the team made use of the largest available brain structure and function dataset across human lifespan: UK Biobank data from 20,000 people aged 50 to 80 years old.
This dataset includes brain scans and brain function measurements and holds data for both healthy individuals and those with a type 2 diabetes diagnosis. The team used this to determine which brain and cognitive changes are specific to diabetes, rather than just aging, and then confirmed these results by comparing them with a meta-analysis of nearly 100 other studies.
Their analysis showed that both aging and type 2 diabetes cause changes in executive functions such as working memory, learning and flexible thinking, and changes in brain processing speed.
However, people with diabetes had a further 13.1% decrease in executive function beyond age-related effects, and their processing speed decreased by a further 6.7% compared to people of the same age without diabetes.
Their meta-analysis of other studies also confirmed this finding: People with type 2 diabetes had consistently and markedly lower cognitive performance compared to healthy individuals who were the same age and similarly educated.
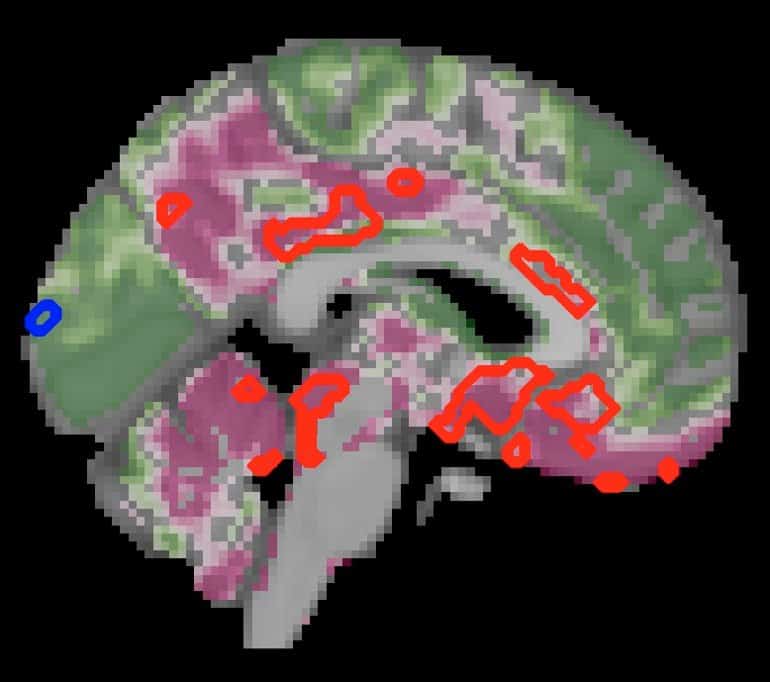
The team also compared brain structure and activity between people with and without diabetes using MRI scans. Here, they found a decrease in gray brain matter with age, mostly in a region called the ventral striatum—which is critical to the brain’s executive functions.
Yet people with diabetes had even more pronounced decreases in gray matter beyond the typical age-related effects—a further 6.2% decrease in gray matter in the ventral striatum, but also loss of gray matter in other regions, compared with normal aging.
Together, the results suggest that the patterns of type 2 diabetes-related neurodegeneration strongly overlap with those of normal aging, but that neurodegeneration is accelerated.
Moreover, these effects on brain function were more severe with increased duration of diabetes. In fact, progression of diabetes was linked with a 26% acceleration of brain aging.
“Our findings suggest that type 2 diabetes and its progression may be associated with accelerated brain aging, potentially due to compromised energy availability causing significant changes to brain structure and function,” concludes senior author Lilianne Mujica-Parodi, Director of the Laboratory for Computational Neurodiagnostics, Stony Brook University.
“By the time diabetes is formally diagnosed, this damage may already have occurred. But brain imaging could provide a clinically valuable metric for identifying and monitoring these neurocognitive effects associated with diabetes.
“Our results underscore the need for research into brain-based biomarkers for type 2 diabetes and treatment strategies that specifically target its neurocognitive effects.”
About this diabetes and brain aging research news
Author: Emily Packer
Source: eLife
Contact: Emily Packer – eLife
Image: The image is credited to Lilianne Mujica-Parodi
Original Research: Open access.
“Type 2 diabetes mellitus accelerates brain aging and cognitive decline: Complementary findings from UK Biobank and meta-analyses” by Botond Antal et al. eLife
Abstract
Type 2 diabetes mellitus accelerates brain aging and cognitive decline: Complementary findings from UK Biobank and meta-analyses
Background: Type 2 diabetes mellitus is known to be associated with neurobiological and cognitive deficits; however, their extent, overlap with aging effects, and the effectiveness of existing treatments in the context of the brain are currently unknown.
Methods: We characterized neurocognitive effects independently associated with T2DM and age in a large cohort of human subjects from the UK Biobank with cross-sectional neuroimaging and cognitive data. We then proceeded to evaluate the extent of overlap between the effects related to T2DM and age by applying correlation measures to the separately characterized neurocognitive changes.
Our findings were complemented by meta-analyses of published reports with cognitive or neuroimaging measures for T2DM and healthy controls (HC). We also evaluated in a cohort of T2DM diagnosed individuals using UK Biobank how disease chronicity and metformin treatment interact with the identified neurocognitive effects.
Results: The UK Biobank dataset included cognitive and neuroimaging data (N=20,314) including 1,012 T2DM and 19,302 HC, aged between 50 and 80 years. Duration of T2DM ranged from 0-31 years (mean 8.5±6.1 years); 498 were treated with metformin alone, while 352 were unmedicated. Our meta-analysis evaluated 34 cognitive studies (N=22,231) and 60 neuroimaging studies: 30 of T2DM (N=866) and 30 of aging (N=1,088).
As compared to age, sex, education, and hypertension-matched HC, T2DM was associated with marked cognitive deficits, particularly in executive functioning and processing speed. Likewise, we found that the diagnosis of T2DM was significantly associated with gray matter atrophy, primarily within the ventral striatum, cerebellum, and putamen, with reorganization of brain activity (decreased in the caudate and premotor cortex and increased in the subgenual area, orbitofrontal cortex, brainstem and posterior cingulate cortex).
The structural and functional changes associated with T2DM show marked overlap with the effects correlating with age but appear earlier, with disease duration linked to more severe neurodegeneration. Metformin treatment status was not associated with improved neurocognitive outcomes.
Conclusions: The neurocognitive impact of T2DM suggests marked acceleration of normal brain aging. T2DM gray matter atrophy occurred approximately 26% ± 14% faster than seen with normal aging; disease duration was associated with increased neurodegeneration. Mechanistically, our results suggest a neurometabolic component to brain aging. Clinically, neuroimaging-based biomarkers may provide a valuable adjunctive measure of T2DM progression and treatment efficacy based on neurological effects.
Funding: The research described in this paper was funded by the W. M. Keck Foundation (to LRMP), the White House Brain Research Through Advancing Innovative Technologies (BRAIN) Initiative (NSFNCS-FR 1926781 to LRMP), and the Baszucki Brain Research Fund (to LRMP). None of the funding sources played any role in the design of the experiments, data collection, analysis, interpretation of the results, the decision to publish, or any aspect relevant to the study. DJW reports serving on data monitoring committees for Novo Nordisk. None of the authors received funding or in-kind support from pharmaceutical and/or other companies to write this manuscript.






