A new study has found a “significant association” between adults who have suffered a traumatic brain injury at some point in their lives and who also have attention deficit hyperactive disorder.
The study, published today in the Journal of Psychiatric Research, supports research that found a similar association in children, said Dr. Gabriela Ilie, lead author of the study and a post-doctoral fellow at St. Michael’s Hospital.
The data used in the adult study was collected by the Centre for Addiction and Mental Health’s Monitor, a continuous, cross-sectional telephone survey of almost 4,000 Ontario residents age 18 and older. Traumatic brain injury was described as any injury to the head that resulted in loss of consciousness for at least five minutes or overnight hospitalization. ADHD was measured by self-reported history of an ADHD diagnosis or the Adult ADHD Self-Report Scale known as the ASRS.
Among adults with a history of TBI, 5.9 per cent reported having been diagnosed with ADHD in their lifetime and another 6.6 per cent screened positive for ADHD when the self-report scale was conducted during the phone survey.
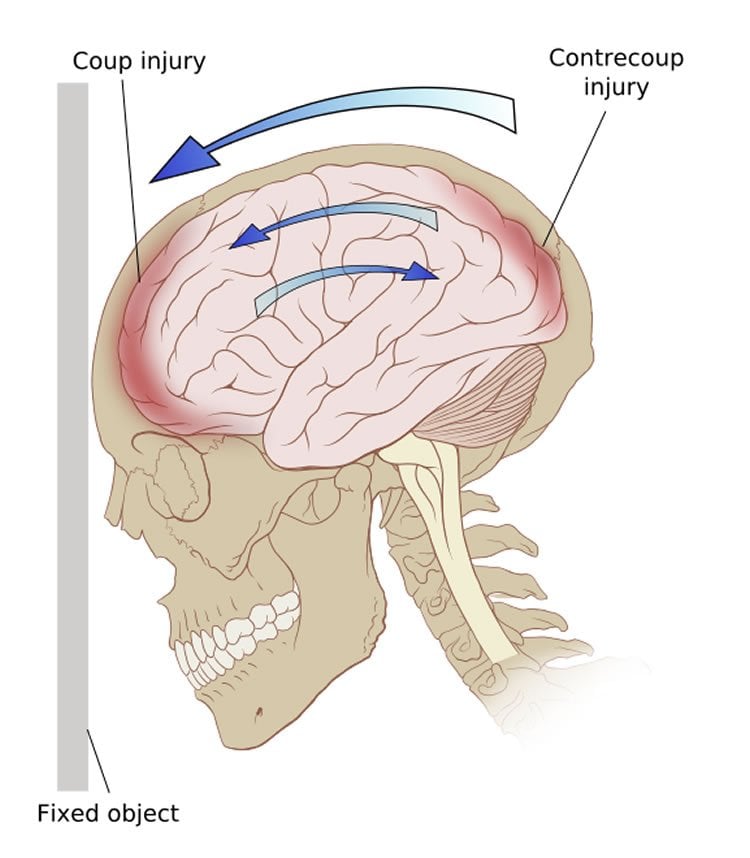
Recent clinical studies have suggested a relationship between ADHD and TBI that were experienced in childhood. “This is not surprising because some of the most persistent consequences of TBI include ADHD-like symptoms, such as memory and attention impairment, deficits in executive functions such as planning and organization, processing consonants and vowels and impulsive behaviour,” Dr. Ilie said.
Other studies have suggested that TBI may lead to psycho-neurological changes that facilitate ADHD or ADHD may increase the probability that a person may fall or have another accident that will result in a TBI.
“Therefore it may be useful to assess TBI history during screening and assessment of ADHD in the adult population,” Dr. Ilie said.
Dr. Robert Mann, senior scientist at CAMH and co-principal investigator said this latest study extends previous findings from the research team about the association between TBI and mental health and addiction issues.
“These new data suggest a significant association between ADHD and TBI,” Dr. Mann said. “We see that adults with TBI are more than twice as likely than those without to report symptoms of ADHD.”
Traumatic brain injuries are increasing in developed countries. The World Health Organization has predicted that by 2020 TBI will become the third largest contributor of disease and disability in the world, following heart disease and depressions.
Injuries from team sports such as hockey and football have been identified as the main source of TBI among youth, while falls and motor vehicle collisions are the main causes among adults.
Funding: This work was financially supported by the Canadian Institutes of Health Research and by the Ontario Neurotrauma Foundation. Additional funding was obtained from AUTO21, a member of the Networks of Centres of Excellence program that is administered and funded by the Natural Sciences and Engineering Research Council, the Canadian Institutes of Health Research, and the Social Sciences and Humanities Research Council, in partnership with Industry Canada.
Source: Leslie Shepherd – St. Michael’s Hospital
Image Credit: The image is credited to Patrick J. Lynch and is licensed CC BY 2.5
Original Research: Abstract for “The association between traumatic brain injury and ADHD in a Canadian adult sample” by Gabriela Ilie, PhD, Evelyn R. Vingilis, PhD, Robert E. Mann, PhD, Hayley Hamilton, PhD, Maggie Toplak, PhD, Edward M. Adlaf, PhD, Nathan Kolla, PhD, Anca Ialomiteanu, MSc, Mark van der Mass, PhD, Mark Asbridge, PhD, Larissa Vingilis-Jaremko, PhD, Jürgen Rehm, PhD, and Michael D. Cusimano, PhD in Journal of Psychiatric Research. Published online August 7 2015 doi:10.1016/j.jpsychires.2015.08.004
Abstract
The association between traumatic brain injury and ADHD in a Canadian adult sample
Highlights
•This study examined the relationship between brain injury and adult attention deficit disorder.
•Results indicate that among brain injured adults a significant proportion have a history of ADHD.
•Among brain injured adults a significant proportion of them screen positive for ADHD.
•Improved screening for ADHD are needed for adults with a history of brain injuries.
Objective
This study describes the association between lifetime traumatic brain injury (TBI) and attention deficit and hyperactivity disorder (ADHD) among Canadian adults.
Method
A cross-sectional sample of 3,993 Ontario adults aged 18 or older were surveyed by Computer Assisted Telephone Interviewing (CATI) throughout 2011 and 2012 as part of the CAMH Monitor, a rolling survey assessing the health, mental health and substance use of Ontario adults aged 18 and older. TBI was defined as trauma to the head that resulted in loss of consciousness for at least five minutes or overnight hospitalization. ADHD was measured by the 6-item ASRS screener for adult ADHD, and self-reported history of diagnosed ADHD.
Results
Among adults with a history of TBI, 6.6% (95% CI: 4.7, 9.4) screened ADHD positive, and 5.9% (95% CI: 3.6, 9.5) reported having been diagnosed with ADHD in their lifetime. Adults with lifetime TBI had significantly greater odds of scoring positive on the ADHD/ASRS screen (OR=2.49, 95% CI: 1.54, 4.04), and of reporting a history of diagnosed ADHD (OR=2.64, 95% CI: 1.40, 4.98) than without TBI, when holding values of sex, age, and education constant.
Conclusion
Significant positive associations between lifetime TBI and both current and past ADHD were observed among adults in this population. More research to understand these associations, and their significance for the etiology and management of TBI and ADHD, is needed.
“The association between traumatic brain injury and ADHD in a Canadian adult sample” by Gabriela Ilie, PhD, Evelyn R. Vingilis, PhD, Robert E. Mann, PhD, Hayley Hamilton, PhD, Maggie Toplak, PhD, Edward M. Adlaf, PhD, Nathan Kolla, PhD, Anca Ialomiteanu, MSc, Mark van der Mass, PhD, Mark Asbridge, PhD, Larissa Vingilis-Jaremko, PhD, Jürgen Rehm, PhD, and Michael D. Cusimano, PhD in Journal of Psychiatric Research. Published online August 7 2015 doi:10.1016/j.jpsychires.2015.08.004