Summary: Researchers report people with sleep apnea have trouble recalling details of autobiographical memories, putting them at greater risk of developing depression.
Source: RMIT Memory.
People with sleep apnea struggle to remember details of memories from their own lives, potentially making them vulnerable to depression, new research has shown.
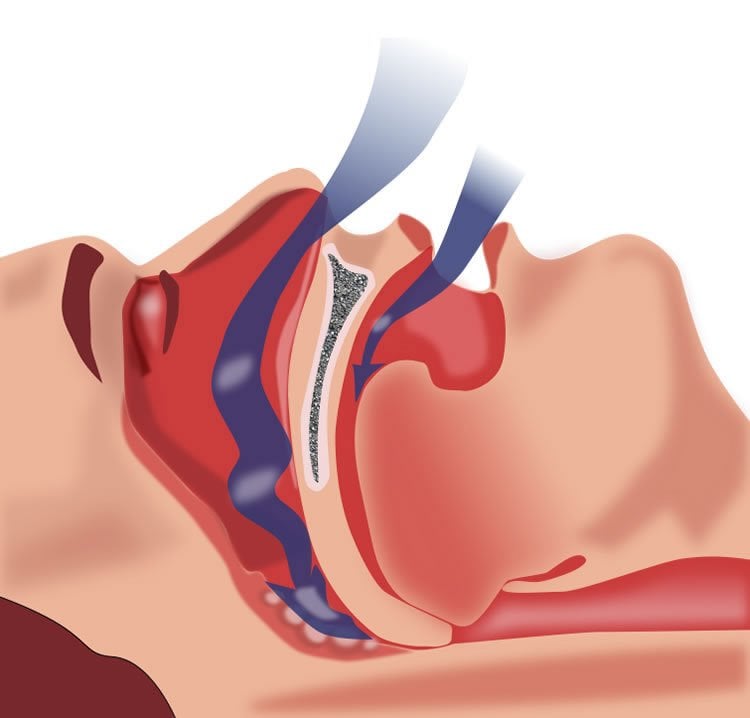
Estimated to affect more than 936 million people worldwide*, obstructive sleep apnea (OSA) is a serious condition that occurs when a person’s breathing is interrupted during sleep.
People with OSA are known to suffer memory problems and also have higher rates of depression but it is not well understood how these issues are connected with the development of the disease.
The new study led by RMIT University in Melbourne, Australia, examined how the condition affected autobiographical memory and found people with untreated OSA had problems recalling specific details about their lives.
Lead investigator Dr Melinda Jackson said the research built on the known links between depression and memory.
“We know that overly general autobiographical memories – where people don’t remember many specific details of life events – are associated with the development of persistent depression,” Jackson said.
“Our study suggests sleep apnoea may impair the brain’s capacity to either encode or consolidate certain types of life memories, which makes it hard for people to recall details from the past.
“OSA is increasingly common, affecting up to 30% of elderly people and around one in four Australian men aged over 30.
“Sleep apnoea is also a significant risk factor for depression so if we can better understand the neurobiological mechanisms at work, we have a chance to improve the mental health of millions of people.”
The study compared 44 adults with untreated OSA to 44 healthy controls, assessing their recall of different types of autobiographical memories from their childhood, early adult life and recent life.
The results showed people with OSA had significantly more overgeneral memories – 52.3% compared with 18.9% of the control group.
The study also looked at recall of semantic memory (facts and concepts from your personal history, like the names of your school teachers) and episodic memory (events or episodes, like your first day of high school).
While people with OSA struggled with semantic memory, their episodic memory was preserved. This is likely related to their fragmented sleeping patterns, as research has shown that good sleep is essential for the consolidation of semantic autobiographical memory.
Across both groups, being older was associated with having a higher number of overgeneral autobiographical memories while higher depression was linked to having worse semantic memory.
Jackson, a Vice-Chancellor’s Senior Research Fellow in RMIT’s School of Biomedical and Health Sciences, said the results showed the need for further studies to better understand the role of untreated OSA on memory processing.
“Brain scans of people with sleep apnoea show they have a significant loss of grey matter from regions that overlap with the autobiographic memory network,” she said.
“We need to look at whether there’s a shared neurobiological mechanism at work – that is, does the dysfunction of that network lead to both depression and memory problems in people with sleep apnoea?”
Jackson said the use of CPAP machines to treat OSA had been shown to improve some of the cognitive impairments related to the condition.
“An important next step will be to determine whether successful treatment of sleep apnoea can also help counter some of these memory issues or even restore the memories that have been lost.”
Source: Gosia Kaszubska – RMIT Memory
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Abstract for “Autobiographical Memory From Different Life Stages in Individuals With Obstructive Sleep Apnea” by Neha Delhikar, Lucy Sommers, Genevieve Rayner, Rachel Schembri, Stephen R. Robinson, Sarah Wilson and Melinda L. Jackson in Journal of the International Neuropsychology Society. Published January 30 2019.
doi:10.1017/S1355617718001091
[cbtabs][cbtab title=”MLA”]RMIT Memory”Sleep Apnea Creates Gaps in Life Memories.” NeuroscienceNews. NeuroscienceNews, 31 January 2019.
<https://neurosciencenews.com/sleep-apnea-memory-10668/>.[/cbtab][cbtab title=”APA”]RMIT Memory(2019, January 31). Sleep Apnea Creates Gaps in Life Memories. NeuroscienceNews. Retrieved January 31, 2019 from https://neurosciencenews.com/sleep-apnea-memory-10668/[/cbtab][cbtab title=”Chicago”]RMIT Memory”Sleep Apnea Creates Gaps in Life Memories.” https://neurosciencenews.com/sleep-apnea-memory-10668/ (accessed January 31, 2019).[/cbtab][/cbtabs]
Abstract
Autobiographical Memory From Different Life Stages in Individuals With Obstructive Sleep Apnea
Objectives: Autobiographical memory dysfunction is a marker of vulnerability to depression. Patients with obstructive sleep apnea (OSA) experience high rates of depression and memory impairment, and autobiographical memory impairments have been observed compared to healthy controls; however, these groups were not age-matched. This study aimed to determine whether individuals with untreated OSA have impaired autobiographical memory when compared to age-matched controls, and to assess the quality of autobiographical memories from three broad time points.
Methods: A total of 44 participants with OSA (M age=49.4±13.0) and 44 age-matched controls (M age=50.0±13.1) completed the Autobiographical Memory Interview (AMI) to assess semantic and episodic memories from three different life stages, and 44 OSA participants and 37 controls completed the Autobiographical Memory Test (AMT) to assess overgeneral memory recall (an inability to retrieve specific memories).
Results: OSA participants had significantly poorer semantic recall of early adult life on the AMI (p<.001), and more overgeneral autobiographical memories recalled on the AMT (=.001), than controls. Poor semantic recall from early adult life was significantly correlated with more depressive symptoms (p=0.006) and lower education (p<0.02), while higher overgeneral memory recall was significantly associated with older age (p=.001).
Conclusions: A specific deficit in semantic autobiographical recall was observed in individuals with OSA. OSA patients recalled more overgeneral memories, suggesting that aspects of the sleep disorder affect their ability to recollect specific details of events from their life. These cognitive features of OSA may contribute to the high incidence of depression in this population.







