Summary: Researchers have developed a new neural interface that is able to relay commands from the central nervous system to a robotic prosthesis.
Source: MIT.
Humans can accurately sense the position, speed, and torque of their limbs, even with their eyes shut. This sense, known as proprioception, allows humans to precisely control their body movements.
Despite significant improvements to prosthetic devices in recent years, researchers have been unable to provide this essential sensation to people with artificial limbs, limiting their ability to accurately control their movements.
Researchers at the Center for Extreme Bionics at the MIT Media Lab have invented a new neural interface and communication paradigm that is able to send movement commands from the central nervous system to a robotic prosthesis, and relay proprioceptive feedback describing movement of the joint back to the central nervous system in return.
This new paradigm, known as the agonist-antagonist myoneural interface, involves a novel surgical approach to limb amputation in which dynamic muscle relationships are preserved within the amputated limb. The AMI was validated in extensive preclinical experimentation at MIT prior to its first surgical implementation in a human patient at Brigham and Women’s Faulkner Hospital.
In a paper published today in Science Translational Medicine, the researchers describe the first human implementation of the agonist-antagonist myoneural interface (AMI), in a person with below-knee amputation.
The paper represents the first time information on joint position, speed, and torque has been fed from a prosthetic limb into the nervous system, according to senior author and project director Hugh Herr, a professor of media arts and sciences at the MIT Media Lab.
“Our goal is to close the loop between the peripheral nervous system’s muscles and nerves, and the bionic appendage,” says Herr.
To do this, the researchers used the same biological sensors that create the body’s natural proprioceptive sensations.
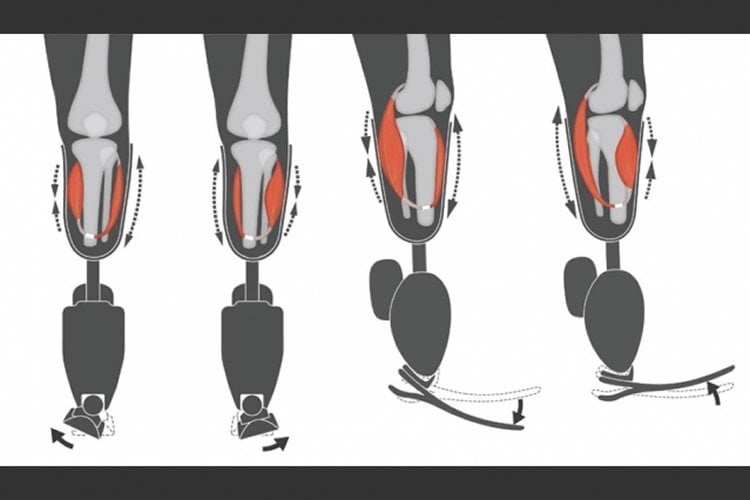
The AMI consists of two opposing muscle-tendons, known as an agonist and an antagonist, which are surgically connected in series so that when one muscle contracts and shortens — upon either volitional or electrical activation — the other stretches, and vice versa.
This coupled movement enables natural biological sensors within the muscle-tendon to transmit electrical signals to the central nervous system, communicating muscle length, speed, and force information, which is interpreted by the brain as natural joint proprioception.
This is how muscle-tendon proprioception works naturally in human joints, Herr says.
“Because the muscles have a natural nerve supply, when this agonist-antagonist muscle movement occurs information is sent through the nerve to the brain, enabling the person to feel those muscles moving, both their position, speed, and load,” he says.
By connecting the AMI with electrodes, the researchers can detect electrical pulses from the muscle, or apply electricity to the muscle to cause it to contract.
“When a person is thinking about moving their phantom ankle, the AMI that maps to that bionic ankle is moving back and forth, sending signals through the nerves to the brain, enabling the person with an amputation to actually feel their bionic ankle moving throughout the whole angular range,” Herr says.
Decoding the electrical language of proprioception within nerves is extremely difficult, according to Tyler Clites, first author of the paper and graduate student lead on the project.
“Using this approach, rather than needing to speak that electrical language ourselves, we use these biological sensors to speak the language for us,” Clites says. “These sensors translate mechanical stretch into electrical signals that can be interpreted by the brain as sensations of position, speed, and force.”
The AMI was first implemented surgically in a human patient at Brigham and Women’s Faulkner Hospital, Boston, by Matthew Carty, one of the paper’s authors, a surgeon in the Division of Plastic and Reconstructive Surgery, and an MIT research scientist.
In this operation, two AMIs were constructed in the residual limb at the time of primary below-knee amputation, with one AMI to control the prosthetic ankle joint, and the other to control the prosthetic subtalar joint.
“We knew that in order for us to validate the success of this new approach to amputation, we would need to couple the procedure with a novel prosthesis that could take advantage of the additional capabilities of this new type of residual limb,” Carty says. “Collaboration was critical, as the design of the procedure informed the design of the robotic limb, and vice versa.”
Toward this end, an advanced prosthetic limb was built at MIT and electrically linked to the patient’s peripheral nervous system using electrodes placed over each AMI muscle following the amputation surgery.
The researchers then compared the movement of the AMI patient with that of four people who had undergone a traditional below-knee amputation procedure, using the same advanced prosthetic limb.
They found that the AMI patient had more stable control over movement of the prosthetic device and was able to move more efficiently than those with the conventional amputation. They also found that the AMI patient quickly displayed natural, reflexive behaviors such as extending the toes toward the next step when walking down a set of stairs.
These behaviors are essential to natural human movement and were absent in all of the people who had undergone a traditional amputation.
What’s more, while the patients with conventional amputation reported feeling disconnected to the prosthesis, the AMI patient quickly described feeling that the bionic ankle and foot had become a part of their own body.
“This is pretty significant evidence that the brain and the spinal cord in this patient adopted the prosthetic leg as if it were their biological limb, enabling those biological pathways to become active once again,” Clites says. “We believe proprioception is fundamental to that adoption.”
It is difficult for an individual with a lower limb amputation to gain a sense of embodiment with their artificial limb, according to Daniel Ferris, the Robert W. Adenbaum Professor of Engineering Innovation at the University of Florida, who was not involved in the research.
“This is ground breaking. The increased sense of embodiment by the amputee subject is a powerful result of having better control of and feedback from the bionic limb,” Ferris says. “I expect that we will see individuals with traumatic amputations start to seek out this type of surgery and interface for their prostheses — it could provide a much greater quality of life for amputees.”
The researchers have since carried out the AMI procedure on nine other below-knee amputees and are planning to adapt the technique for those needing above-knee, below-elbow, and above-elbow amputations.
“Previously, humans have used technology in a tool-like fashion,” Herr says. “We are now starting to see a new era of human-device interaction, of full neurological embodiment, in which what we design becomes truly part of us, part of our identity.”
Source: Helen Knight – MIT
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is credited to MIT Media Lab/Biomechatronics group. Original artwork by Stephanie Ku.
Original Research: Abstract for “Proprioception from a neurally controlled lower-extremity prosthesis” by Tyler R. Clites, Matthew J. Carty, Jessica B. Ullauri, Matthew E. Carney, Luke M. Mooney, Jean-François Duval, Shriya S. Srinivasan and Hugh. M. Herr in Science Translational Medicine. Published May 30 2018.
doi:10.1126/scitranslmed.aap8373
[cbtabs][cbtab title=”MLA”]MIT “Surgical Technique Improves Sensation and Control of Prosthetic Limbs.” NeuroscienceNews. NeuroscienceNews, 2 June 2018.
<https://neurosciencenews.com/prosthetic-limb-sensation-9218/>.[/cbtab][cbtab title=”APA”]MIT (2018, June 2). Surgical Technique Improves Sensation and Control of Prosthetic Limbs. NeuroscienceNews. Retrieved June 2, 2018 from https://neurosciencenews.com/prosthetic-limb-sensation-9218/[/cbtab][cbtab title=”Chicago”]MIT “Surgical Technique Improves Sensation and Control of Prosthetic Limbs.” https://neurosciencenews.com/prosthetic-limb-sensation-9218/ (accessed June 2, 2018).[/cbtab][/cbtabs]
Abstract
Proprioception from a neurally controlled lower-extremity prosthesis
Humans can precisely sense the position, speed, and torque of their body parts. This sense is known as proprioception and is essential to human motor control. Although there have been many attempts to create human-mechatronic interactions, there is still no robust, repeatable methodology to reflect proprioceptive information from a synthetic device onto the nervous system. To address this shortcoming, we present an agonist-antagonist myoneural interface (AMI). The AMI is composed of (i) a surgical construct made up of two muscle-tendons—an agonist and an antagonist—surgically connected in series so that contraction of one muscle stretches the other and (ii) a bidirectional efferent-afferent neural control architecture. The AMI preserves the dynamic muscle relationships that exist within native anatomy, thereby allowing proprioceptive signals from mechanoreceptors within both muscles to be communicated to the central nervous system. We surgically constructed two AMIs within the residual limb of a subject with a transtibial amputation. Each AMI sends control signals to one joint of a two-degree-of-freedom ankle-foot prosthesis and provides proprioceptive information pertaining to the movement of that joint. The AMI subject displayed improved control over the prosthesis compared to a group of four subjects having traditional amputation. We also show natural reflexive behaviors during stair ambulation in the AMI subject that do not appear in the cohort of subjects with traditional amputation. In addition, we demonstrate a system for closed-loop joint torque control in AMI subjects. These results provide a framework for integrating bionic systems with human physiology.






