Summary: Mindfulness-based stress reduction can help reduce symptoms of neuropathic pain in breast cancer survivors.
Source: University of Ottawa
A study led by University of Ottawa researchers provides empirical evidence that mindfulness has a significant impact on the brain of women suffering from neuropathic pain related to breast cancer treatment. The researchers showed that mindfulness-based stress reduction (MBSR) helps modulate neuropathic pain.
Their findings could make a difference in the lives of many women. In Canada, over a quarter of a million women are expected to be diagnosed with breast cancer – the most diagnosed cancer among women worldwide – in 2020. In addition to the psychological impacts of breast cancer, approximately 20 to 50 percent of survivors report experiencing chronic neuropathic pain following treatment.
We talked to senior author Dr. Andra Smith, Full Professor at the uOttawa School of Psychology, to learn more about the most recent findings published in the journal Mindfulness.
Why did you and your team decide to look at mindfulness to improve pain-related problems?
“Neuropathic pain is a very common side effect of chemotherapy and other breast cancer treatments. Pain killers do not always work and quality of life, cognitive abilities, and overall well-being can be reduced due to this pain. Due to these negative effects and the complexity of treatment for this type of pain following breast cancer treatment, it is important to provide adjunct treatment and management options.
We have heard a lot about mindfulness over the past few years, about how it helps people relax and feel better. If mindfulness, a non-pharmacological tool, can be used to help with neuropathic pain, women will feel better and might not experience such disruptive pain.
Pain is a subjective experience and mindfulness is often dismissed as a “buzz word.” But our research provides objective, empirical evidence of a significant impact of mindfulness on the brain of these women.”
How was the research conducted?
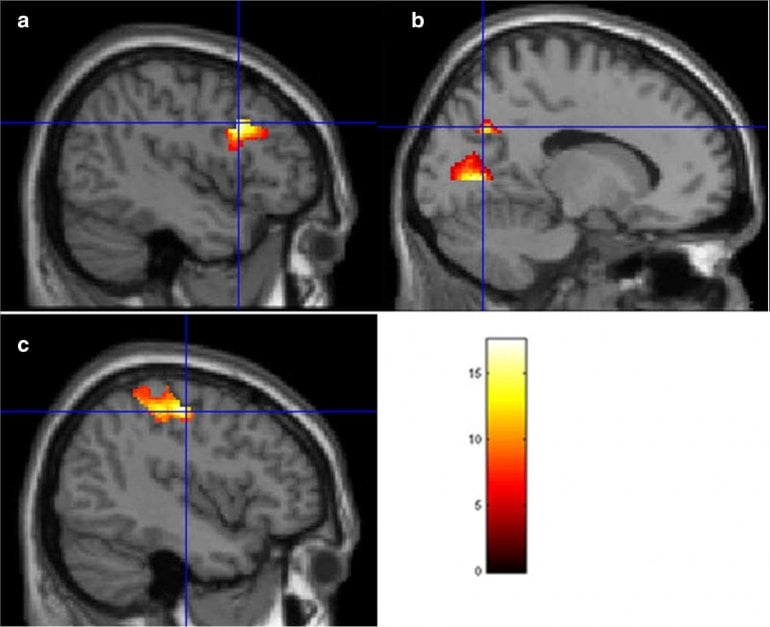
“We investigated the impact of an 8-week mindfulness-based stress reduction (MBSR) program on emotional reactivity among a sample of breast cancer survivors with chronic neuropathic pain. We used state-of-the-art brain imaging at The Ottawa Hospital, on their 3T MRI scanner and collected data on white matter health, brain activity during emotional pain related word processing and during resting state.
Women with neuropathic pain were imaged before and after an MBSR program, or treatment as usual. Pain, quality of life, and imaging were compared between the two groups and within the MBSR group pre- and post-MBSR.”
What did you find?
“We observed major reductions in brain activity following mindfulness-based stress reduction in regions related to pain, emotional regulation, and cognitive processing. Both pain severity and pain interference, for the MBSR group, were significantly reduced after the 8-week training.
Our results show a significant improvement in brain health as well as in pain perception.
There are many anecdotal reports of how this or that made a person “feel better” but the really exciting results here are that we can see that there are actual changes in the brain and the way a person can alter their response to pain.”
Why is it important?
“This research provides hope for a non-invasive method of easing the struggle of chronic neuropathic pain in women following breast cancer treatment.
Pain is something that people fear, and many people run into significant secondary problems because of their pain medication use, including drug misuse and mental health issues. Mindfulness has a neurophysiological effect that can alter one’s perception of pain.
This research shows that there are adjunctive treatment options. If used properly, the information we have published can improve health outcomes for the people involved and could potentially also reduce health costs, as well as some of the related problems – particularly those related to mental health.”
Who worked on this research?
“Dr. Patricia Poulin, at The Ottawa Hospital, was the clinical principal investigator with her research team of Heather Romanow, Yaad Shergill, Emily Tennant, and Eve-Ling Khoo. This included recruitment of the women and all clinical assessments.
My lab performed the scanning component of the study, including my imaging team of Dr. Taylor Hatchard, Ola Mioduszewski and Dr. Lydia Fang.
The data was collected over two years, from 2017 to 2019, funded by both Canadian Institutes of Health Research (CIHR) and Canadian Breast Cancer Foundation grants. We published three articles on our research in the last four months.
About this cancer and pain research news
Source: University of Ottawa
Contact: Justine Boutet – University of Ottawa
Image: The image is credited to University of Ottawa
Original Research: Closed access.
“Reduced Emotional Reactivity in Breast Cancer Survivors with Chronic Neuropathic Pain Following Mindfulness-Based Stress Reduction (MBSR): an fMRI Pilot Investigation” by Taylor Hatchard, Ola Mioduszewski, Eve-Ling Khoo, Heather Romanow, Yaad Shergill, Emily Tennant, Allison Leeming, Zhuo Fang, Patricia Poulin & Andra M. Smith. Mindfulness
Abstract
Reduced Emotional Reactivity in Breast Cancer Survivors with Chronic Neuropathic Pain Following Mindfulness-Based Stress Reduction (MBSR): an fMRI Pilot Investigation
Objectives
The present study aimed to investigate the impact of an 8-week mindfulness-based stress reduction (MBSR) program on emotional reactivity among a sample of breast cancer survivors with chronic neuropathic pain (CNP).
Methods
Twenty-one women were randomly assigned to a MBSR treatment group (n = 11) or a waitlist control group (n = 10) following medical review. Using functional magnetic resonance imaging (fMRI), participants were imaged before and after the MBSR program while completing the emotional Stroop task as a measure of emotional reactivity.
Results
The treatment group showed significantly less blood oxygen level–dependent (BOLD) activity post-MBSR across several brain regions involved in pain processing and visual attention. This included regions in the left somatosensory cortex, left precuneus, and left dorsolateral prefrontal cortex. Although emotional reactivity was the primary outcome, pain severity and interference from the Brief Pain Inventory were also assessed at both time points. Pain interference was significantly reduced following MBSR for the intervention group only.
Conclusions
These preliminary findings show that MBSR training has a marked impact on neural correlates of pain processing and attention, lending support to MBSR as a viable adjunctive treatment option for breast cancer survivors living with CNP. However, further research, with a larger sample size, is warranted.






