The results of a new study suggest that nocturnal enuresis, or bedwetting, may be an additional symptom that doctors can look for when assessing post-menopausal women for obstructive sleep apnea. That condition left untreated can lead to serious medical problems, such as cardiovascular disease, as organs are undersupplied with oxygen.
About 2 percent of women reportedly experience OSA, but it may be underdiagnosed among older women, said Dr. Patrick Koo, lead author of the new study in the journal Menopause. Past research suggests that women may understate some symptoms when reporting poor sleep, leading to misdiagnoses of depression or insomnia. Koo, a clinical assistant professor of medicine in the Alpert Medical School of Brown University and a physician at Memorial Hospital of Rhode Island, therefore set out to determine whether nocturnal enuresis, which has been associated with OSA in children, might be an additional risk factor worth considering.
To do that he and his co-authors analyzed the vast trove of health data compiled by the Women’s Health Initiative, a massive research program that enrolled and followed more than 161,000 post-menopausal women between 1993 and 2005. Koo and his colleagues were able to review the prevalence of traditional OSA risk factors among the women – obesity, snoring, poor sleep, interrupted sleep, hypertension, daytime sleepiness – and their individual and collective association with nocturnal enuresis. In the analysis they accounted for a wide range of possible confounding factors, including the number of term pregnancies, alcohol consumption, and many other demographic and medical characteristics.
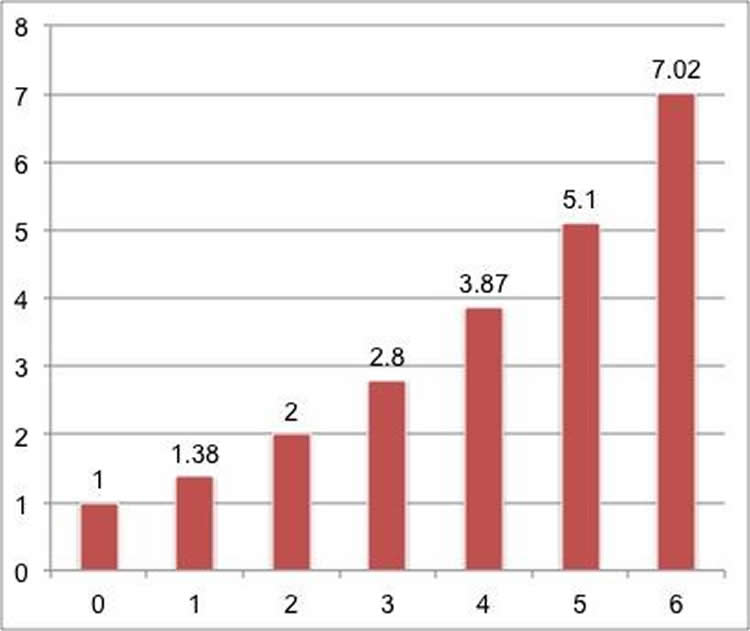
What they found is that the more traditional OSA risk factors a woman experienced, the greater the odds that she also experienced nocturnal enuresis. A woman with any two OSA risk factors, for example, was on average twice as likely as a woman with none to urinate in her sleep. A woman with four OSA risk factors was nearly four times as likely.
“We demonstrate that OSA risk factors are associated with nocturnal enuresis in postmenopausal women,” Koo and colleagues conclude in the paper. “When screening for OSA, clinicians may find it useful to inquire about nocturnal enuresis as a symptom.”
The study’s corresponding author is Dr. Charles Eaton, a Brown professor of family medicine and of epidemiology. Other authors are Drs. Dennis McCool, Lauren Hale and Katie Stone.
Funding: The National Institutes of Health funded the Women’s Health Initiative.
Source: David Orenstein – Brown University
Image Credit: The image is credited to Brown University
Original Research: Abstract for “Association of obstructive sleep apnea risk factors with nocturnal enuresis in postmenopausal women” by Koo, Patrick; McCool, F. Dennis; Hale, and Lauren; More in Menopause. Published online August 31 2015 doi:10.1097/GME.0000000000000517
Abstract
Association of obstructive sleep apnea risk factors with nocturnal enuresis in postmenopausal women
Objective: The prevalence of obstructive sleep apnea (OSA) in women increases significantly after menopause. However, identifying at-risk women is difficult because they tend to underreport symptoms and their complaints may differ from those traditionally associated with OSA. We investigated whether OSA risk factors are associated with the presence of a “nontraditional” complaint, such as nocturnal enuresis, in postmenopausal women.
Methods: A cross-sectional study of postmenopausal women aged 50 to 79 years who participated in the Women’s Health Initiative Observational Study and clinical trials (1993-2005) at 40 clinical centers in the United States was performed. Multiple variable logistic regression analysis was used to determine the association of OSA risk factors with nocturnal enuresis.
Results: A cohort of 2,789 women (1.7%) reported having nocturnal enuresis. Obesity (odds ratio [OR], 2.29; 95% CI, 2.00-2.62), snoring (OR, 2.01; 95% CI, 1.74-2.32), poor sleep quality (OR, 1.70; 95% CI, 1.52-1.91), sleep fragmentation (OR, 2.44; 95% CI, 2.14-2.79), daytime sleepiness (OR, 1.50; 95% CI, 1.33-1.68), and hypertension (OR, 1.13; 95% CI, 1.01-1.26) were associated with nocturnal enuresis. Each additional OSA risk factor in a predefined OSA score significantly increased the odds of having nocturnal enuresis in a dose-response fashion (OR of 1.38, 2.00, 2.80, 3.87, 5.10, and 7.02 for scores of 1-6, respectively) compared with no risk factors.
Conclusions: OSA risk factors are associated with nocturnal enuresis in postmenopausal women. Mechanisms relating nocturnal enuresis to OSA may include apnea-associated changes in intrathoracic pressure, leading to increased urine output. Questioning at-risk postmenopausal women presenting with nocturnal enuresis about other OSA risk factors should be considered.
“Association of obstructive sleep apnea risk factors with nocturnal enuresis in postmenopausal women” by Koo, Patrick; McCool, F. Dennis; Hale, and Lauren; More in Menopause. Published online August 31 2015 doi:10.1097/GME.0000000000000517






