Women with multiple sclerosis (MS) who intended to breastfeed their infants exclusively for two months had a lower risk of relapse during the first six months after giving birth compared with women who did not breastfeed exclusively , according to an article published online by JAMA Neurology.
About 20 percent to 30 percent of women with MS experience a relapse within the first three to four months after giving birth and there are no interventions for effective prevention of postpartum relapse. The effect of exclusive breastfeeding on postpartum risk of MS relapse is controversial with conflicting study results.
Kerstin Hellwig, M.D., of Ruhr-University Bochum, Germany, and coauthors analyzed data from 201 pregnant women with MS collected from 2008 to June 2012 with one-year follow-up postpartum in the nationwide German MS and pregnancy registry. Exclusive breastfeeding was defined as no regular replacement of breastfeeding meals with supplemental feedings for at least two months compared with nonexclusive breastfeeding, which was partial or no breastfeeding.
Of the 201 women, 120 (59.7 percent) intended to breastfeed exclusively for at least two months, 42 women (20.9 percent) combined breastfeeding with supplemental feedings within the first two months after giving birth, and 39 women (19.4 percent) did not breastfeed. Most women [178 (88.6 percent)] had used disease-modifying therapy (DMT) agents before pregnancy.
The authors report that 31 women (38.3 percent) who did not breastfeed exclusively had MS relapse within the first six months postpartum compared with 29 women (24.2 percent) who intended to breastfeed exclusively for at least two months.
The authors note the effect of exclusive breastfeeding “seems to be plausible” since disease activity returned in the second half of the postpartum year in exclusively breastfeeding women, corresponding to the introduction of supplemental feedings and the return of menstruation. The introduction of regular formula feedings or solid food to an infant leads to a change in a woman’s hormonal status resulting in the return to ovulation.
The authors note the main limitation of their study was the selection bias inherent to voluntary registries and reflected in the high proportion of women receiving DMT.
“Taken together, our findings indicate that women with MS should be supported if they choose to breastfeed exclusively since it clearly does not increase the risk of postpartum relapse. Relapse in the first six months postpartum may be diminished by exclusive breastfeeding, but once regular feedings are introduced, disease activity is likely to return,” the study concludes.
Source: Kerstin Hellwig – JAMA Network
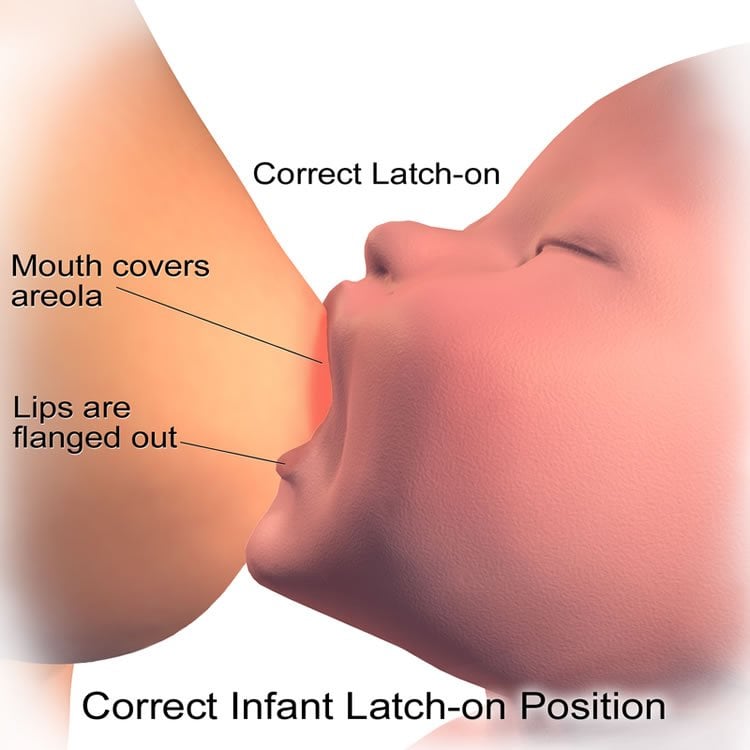
Image Source: The image is credited to Bruce Blaus and is licensed CC BY 3.0
Original Research: Abstract for “Effect of Breastfeeding on Postpartum Multiple Sclerosis Relapse” by Kerstin Hellwig, MD; Milena Rockhoff, MD; Sandra Herbstritt, PharmD; Nadja Borisow, MD; Aiden Haghikia, MD; Birte Elias-Hamp, MD; Sylvia Menck, MD; Ralf Gold, MD; and Annette Langer-Gould, MD, PhD in JAMA Neurology. Published online August 31 2015 doi:10.1001/jamaneurol.2015.1806
Abstract
Effect of Breastfeeding on Postpartum Multiple Sclerosis Relapse
Importance Women with multiple sclerosis (MS) experience an elevated risk of relapse after giving birth. The effect of exclusive breastfeeding on postpartum risk of MS relapse is unclear.
Objectives To determine the effect of exclusive breastfeeding on postpartum risk of MS relapse and to investigate the effect of introducing supplemental feedings on that risk.
Design, Setting, and Participants Data on 201 pregnant women with relapsing-remitting MS were collected prospectively from January 1, 2008, to June 30, 2012, with 1 year follow-up post partum in the nationwide German MS and pregnancy registry. The effect of the intention to breastfeed exclusively (no regular replacement of breastfeeding meals with supplemental feedings) for at least 2 months compared with nonexclusive breastfeeding (partial or no breastfeeding) on the first postpartum MS relapse, using Cox proportional hazards regression model adjusted for age and disease activity, before and during pregnancy was analyzed. Data analysis was performed from August 30, 2013, to May 25, 2015.
Exposure Exclusive breastfeeding defined as at least 2 months of breastfeeding without regular replacement of any meal by supplemental feeding.
Main Outcome and Measure First postpartum MS relapse.
Results Of 201 women, 120 (59.7%) intended to breastfeed exclusively for at least 2 months and 81 (40.3%) breastfed and included supplemental feeding (42 [20.9%]) or did not breastfeed (39 [19.4%]). Thirty-one women (38.3%) who did not breastfeed exclusively had a relapse within the first 6 months post partum compared with 29 women (24.2%) who intended to breastfeed exclusively for at least 2 months (unadjusted hazard ratio, 1.80; 95% CI, 1.09-2.99; P = .02; adjusted hazard ratio, 1.70; 95% CI, 1.02-2.85; P = .04). The time to first postpartum relapse after the introduction of supplemental feedings did not differ significantly between women who previously breastfed exclusively and those who did not (P = .60).
Conclusions and Relevance The findings of this study suggest that exclusive breastfeeding is a modestly effective MS treatment with a natural end date. Our study provides further evidence that women with MS who breastfeed exclusively should be supported to do so since it does not increase the risk of postpartum relapse.
“Effect of Breastfeeding on Postpartum Multiple Sclerosis Relapse” by Kerstin Hellwig, MD; Milena Rockhoff, MD; Sandra Herbstritt, PharmD; Nadja Borisow, MD; Aiden Haghikia, MD; Birte Elias-Hamp, MD; Sylvia Menck, MD; Ralf Gold, MD; and Annette Langer-Gould, MD, PhD in JAMA Neurology. Published online August 31 2015 doi:10.1001/jamaneurol.2015.1806






