Summary: A new study reveals humans and mice have significant differences in how oxidative stress and inflammation trigger immune response genes in astrocytes. Researchers suggest lab models of neurodegeneration should incorporate specially engineered mouse models with lower resistance to oxidative stress, rendering them more human-like.
Source: UCLA
A UCLA-led study comparing brain cells known as astrocytes in humans and mice found that mouse astrocytes are more resilient to oxidative stress, a damaging imbalance that is a mechanism behind many neurological disorders. A lack of oxygen triggers molecular repair mechanisms in these mouse astrocytes but not in human astrocytes. In contrast, inflammation activates immune-response genes in human astrocytes but not mouse astrocytes.
Although the mouse is a ubiquitous laboratory model used in research for neurological diseases, results from studies in mice are not always applicable to humans. In fact, more than 90% of drug candidates that show preclinical promise for neurological disorders ultimately fail when tested in humans, in part due to a dearth of knowledge about the differences in astrocytes and other brain cells between the two species.
Astrocytes are crucial to the development and function of the brain, and they play a substantial role in neurological disorders that, nonetheless, is not fully understood. Injury or infection causes astrocytes to go from a resting to reactive state in which they can aid in repairing the brain but can also increase detrimental inflammation.
The scientists studied developing cells purified from mouse and human brain tissue, as well as cells grown in serum-free cultures from astrocytes selected using an antibody-based method developed by the study’s corresponding author.
This technique was necessary because the conventional method of selecting astrocytes by growing them in serum — a mixture of proteins, hormones, fats and minerals — throws them into a reactive state similar to that caused by infection or injury. With the researchers’ strategy, they were able to examine the astrocytes in a healthy state and in controlled conditions of oxidative stress, lack of oxygen and excessive inflammation.
The findings have implications for basic and translational research into neurological disorders such as Alzheimer’s disease, Parkinson’s disease and amyotrophic lateral sclerosis — conditions whose underlying mechanisms include oxidative stress, lack of oxygen and excessive inflammation.
Because mouse astrocytes stand up to oxidative stress better, the authors suggest that laboratory models for neurodegeneration could be engineered to lessen that resistance, rendering them more human-like. In addition, the mouse astrocyte’s facility for repair in response to lack of oxygen may suggest a new avenue of stroke research.
And neuroscientists can take a more informed approach to preclinical studies by accounting for differences in response to inflammation between mouse and human astrocytes, as well as metabolic differences identified in the study.
Funding: The study was funded by the ARCS Foundation, the National Institutes of Health, the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation, the W. M. Keck Foundation, the Wendy Ablon Trust, a UCLA Broad Stem Cell Research Center Innovation Award and the Friends of the Semel Institute for Neuroscience and Human Behavior at UCLA.
About this neuroscience research news
Source: UCLA
Contact: Tiare Dunlap – UCLA
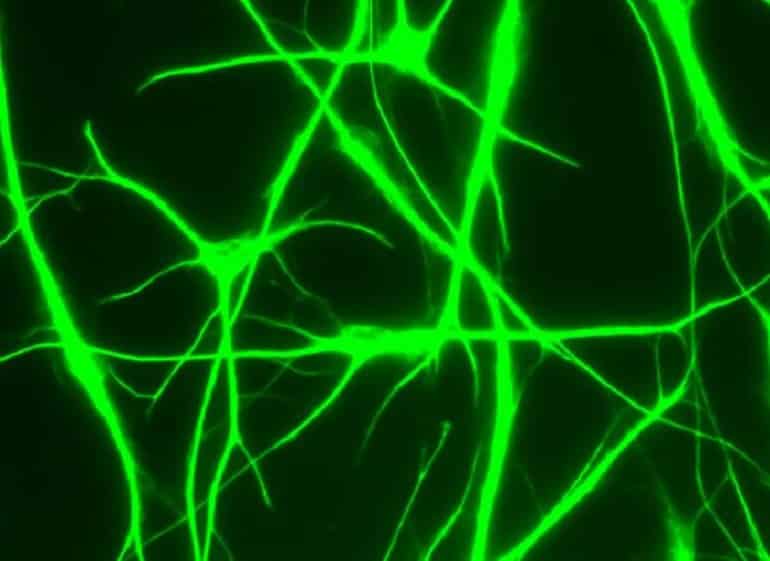
Image: The image is credited to UCLA Broad Stem Cell Research Center/Nature Communications
Original Research: Open access.
“Conservation and divergence of vulnerability and responses to stressors between human and mouse astrocytes” by Jiwen Li, Lin Pan, William G. Pembroke, Jessica E. Rexach, Marlesa I. Godoy, Michael C. Condro, Alvaro G. Alvarado, Mineli Harteni, Yen-Wei Chen, Linsey Stiles, Angela Y. Chen, Ina B. Wanner, Xia Yang, Steven A. Goldman, Daniel H. Geschwind, Harley I. Kornblum & Ye Zhang. Nature Communications
Abstract
Conservation and divergence of vulnerability and responses to stressors between human and mouse astrocytes
Astrocytes play important roles in neurological disorders such as stroke, injury, and neurodegeneration. Most knowledge on astrocyte biology is based on studies of mouse models and the similarities and differences between human and mouse astrocytes are insufficiently characterized, presenting a barrier in translational research.
Based on analyses of acutely purified astrocytes, serum-free cultures of primary astrocytes, and xenografted chimeric mice, we find extensive conservation in astrocytic gene expression between human and mouse samples. However, the genes involved in defense response and metabolism show species-specific differences.
Human astrocytes exhibit greater susceptibility to oxidative stress than mouse astrocytes, due to differences in mitochondrial physiology and detoxification pathways. In addition, we find that mouse but not human astrocytes activate a molecular program for neural repair under hypoxia, whereas human but not mouse astrocytes activate the antigen presentation pathway under inflammatory conditions.
Here, we show species-dependent properties of astrocytes, which can be informative for improving translation from mouse models to humans.






