Summary: A study finds that COVID-19 proteins left in the brain may lower cortisol levels, leading to heightened inflammation and an exaggerated response to stressors.
This discovery could explain the persistent neurological symptoms seen in Long COVID patients. Researchers suggest that managing stressors and investigating viral reservoirs might help alleviate these symptoms.
Key Facts
- COVID-19 proteins in the brain can reduce cortisol by over 30%.
- Lowered cortisol leads to increased brain inflammation and stress response.
- Findings suggest new strategies for managing Long COVID symptoms.
Source: University of Colorado
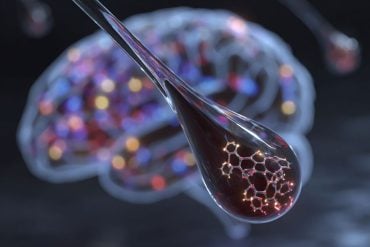
Proteins left behind by COVID-19 long after initial infection can cause cortisol levels in the brain to plummet, inflame the nervous system and prime its immune cells to hyper-react when another stressor arises, according to new animal research by University of Colorado Boulder scientists.
The study, published in the journal Brain Behavior and Immunity, sheds new light on what might underly the neurological symptoms of Long COVID, an intractable syndrome which impacts as many as 35% of those infected with the virus.

The findings come as COVID makes a striking summer comeback, with cases rising in 84 countries and numerous high-profile athletes at the Paris Olympics testing positive.
“Our study suggests that low cortisol could be playing a key role in driving many of these physiological changes that people are experiencing with Long COVID,” said lead author Matthew Frank, PhD, a senior research associate with the Department of Psychology and Neuroscience at CU Boulder.
Previous research has shown that SARS-CoV-2 antigens, immune-stimulating proteins shed by the virus that causes COVID-19, linger in the blood stream of Long COVID patients as much as a year after infection. They’ve also been detected in the brains of COVID patients who have died.
To explore just how such antigens impact the brain and nervous system, the research team injected an antigen called S1 (a subunit of the “spike” protein) into the spinal fluid of rats and compared them to a control group.
After 7 days, in rats exposed to S1, levels of the cortisol-like hormone corticosterone plummeted by 31% in the hippocampus, the region of the brain associated with memory, decision making and learning. After 9 days, levels were down 37%.
“Nine days is a long time in the life span of a rat,” said Frank, noting that rats live on average for two to three years.
He notes that cortisol is a critical anti-inflammatory, helps convert fuel into energy and is important for regulating blood pressure and the sleep-wake cycle and keeping the immune response to infection in check. One recent study showed that people with Long COVID tend to have low cortisol levels. So do people with chronic fatigue syndrome, research shows.
“Cortisol has so many beneficial properties that if it is reduced it can have a host of negative consequences,” said Frank.
In another experiment, the researchers exposed different groups of rats to an immune stressor (a weakened bacteria) and observed their heart rate, temperature and behavior as well as the activity of immune cells in the brain called glial cells.
They found that the group of rats that had previously been exposed to the COVID protein S1 responded far more strongly to the stressor, with more pronounced changes in eating, drinking, behavior, core body temperature and heart rate, more neuroinflammation and stronger activation of glial cells.
“We show for the first time that exposure to antigens left behind by this virus can actually change the immune response in the brain so that it overreacts to subsequent stressors or infection,” said Frank.
He stresses that the study was in animals and that more research is necessary to determine whether and how low cortisol might lead to Long COVID symptoms in people.
But he theorizes that the process might go something like this: COVID antigens lower cortisol, which serves to keep inflammatory responses to stressors in check in the brain. Once a stressor arises – whether it be a bad day at work, a mild infection or a hard workout – the brain’s inflammatory response is unleashed without those limits and serious symptoms come screaming back.
Those might include, fatigue, depression, brain fog, insomnia and memory problems.
Frank said he is doubtful that cortisol treatments alone could be an effective treatment for Long COVID, as they would not get at the root cause and come with a host of side effects.
Instead, the findings suggest that identifying and minimizing different stressors might help manage symptoms.
Rooting out the source of antigens –including tissue reservoirs where bits of virus continue to hide out – might also be an approach worth exploring, he suggests.
The study was funded by the nonprofit PolyBio Research Foundation. More research is underway.
“There are many individuals out there suffering from this debilitating syndrome. This research gets us closer to understanding what, neurobiologically, is going on and how cortisol may be playing a role,” said Frank.
About this long COVID research news
Author: Lisa Marshall
Source: University of Colorado
Contact: Lisa Marshall – University of Colorado
Image: The image is credited to Neuroscience News
Original Research: Open access.
“SARS-CoV-2 S1 subunit produces a protracted priming of the neuroinflammatory, physiological, and behavioral responses to a remote immune challenge: A role for corticosteroids” by Matthew Frank et al. Brain, Behavior, and Immunology
Abstract
SARS-CoV-2 S1 subunit produces a protracted priming of the neuroinflammatory, physiological, and behavioral responses to a remote immune challenge: A role for corticosteroids
Long COVID is a major public health consequence of COVID-19 and is characterized by multiple neurological and neuropsychatric symptoms. SARS-CoV-2 antigens (e.g., spike S1 subunit) are found in the circulation of Long COVID patients, have been detected in post-mortem brain of COVID patients, and exhibit neuroinflammatory properties.
Considering recent observations of chronic neuroinflammation in Long COVID patients, the present study explores the idea that antigens derived from SARS-CoV-2 might produce a long-term priming or sensitization of neuroinflammatory processes, thereby potentiating the magnitude and/or duration of the neuroinflammatory response to future inflammatory insults.
Rats were administered S1 or vehicle intra-cisterna magna and 7d later challenged with vehicle or LPS.
The neuroinflammatory, physiological, and behavioral responses to LPS were measured at various time points post-LPS. We found that prior S1 treatment potentiated many of these responses to LPS suggesting that S1 produces a protracted priming of these processes. Further, S1 produced a protracted reduction in basal brain corticosteroids.
Considering the anti-inflammatory properties of corticosteroids, these findings suggest that S1 might disinhibit innate immune processes in brain by reducing anti-inflammatory drive, thereby priming neuroinflammatory processes.
Given that hypocortisolism is observed in Long COVID, we propose that similar S1-induced innate immune priming processes might play role in the pathophysiology of Long COVID.