Brain plasticity is the ability of the brain to change both anatomically and functionally in response to changes in the body or in the environment.
For many years, researchers believed that the brain did not suffer major changes after childhood. Although brain plasticity predominates in the first years of life, research done in the last 30 years has shown that it may also occur in adulthood, continuing to change through learning. Brain plasticity may also occur following injury, amputation or nerve damage.
Leprosy, also known as Hansen’s disease, can be traced back to early human history. Descriptions of an ailment resembling leprosy as we know it today were found on an Egyptian Papyrus dating back to 1550 B.C. Also, the word tzaraath, which some believe specifically refers to leprosy, can be found in the Old Testament, where it is considered the most dreaded of all diseases.
Leprosy is a chronic infection caused by the bacteria Mycobacterium leprae and Mycobacterium lepromatosis. The bacillus predominantly infects nervous tissues, leading to nervous inflammation that most often affects the eyes, hands and feet. Contamination between individuals may occur through a cough or contact involving fluids. Although currently not very contagious, in the past, patients with leprosy were condemned to live life in isolation in order to save others from the perils of the disease. Leprosy is curable with multidrug therapy but the physical disabilities and deformities remain even after bacteriological cure.
Nerve damage caused by leprosy leads to limb disabilities and deformities such as a claw hand, neuropathic pain and a burning sensation. Patients with leprosy require long-term rehabilitation in order to control the chronic consequences of neural damage. Until now, leprosy was thought to affect the peripheral nerves connecting body parts to the brain without affecting the brain itself. However, a new study done by a multidisciplinary research team at the Federal University of Rio de Janeiro, Brazil, shows that peripheral nerve damage caused by leprosy can indeed change the brain.
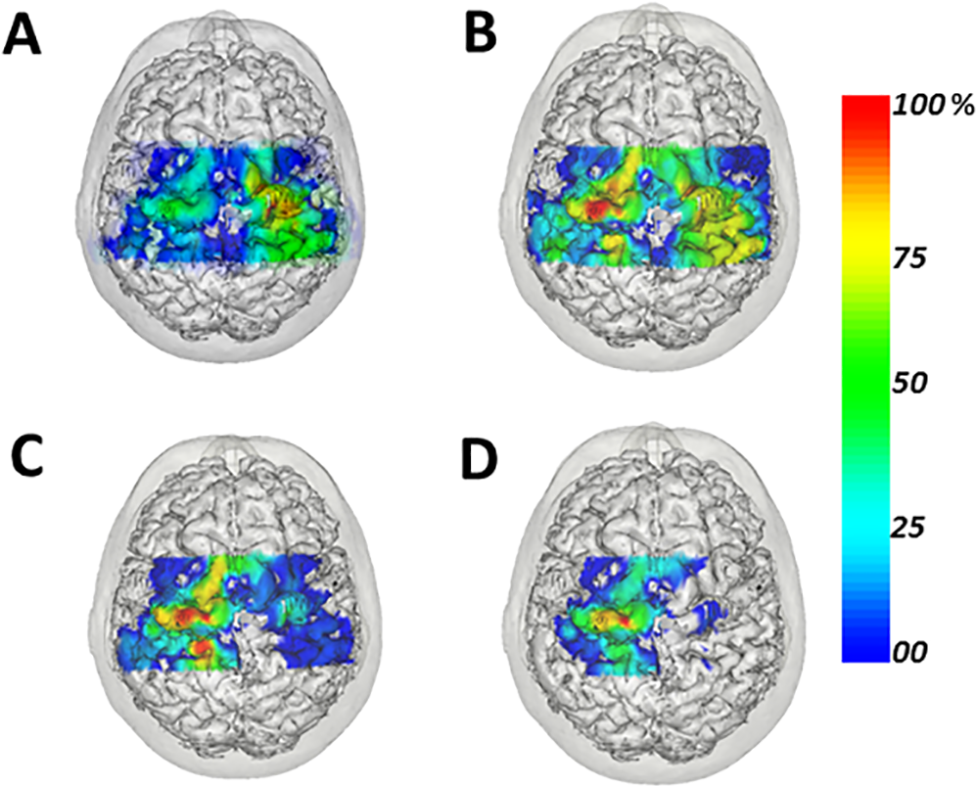
The brain’s motor cortex is the region responsible for generating neural impulses that reach the spinal cord and control the execution of movements. The group led by Dr. Claudia Domingues Vargas used transcranial magnetic stimulation (TMS), a noninvasive method, to measure the connection between the brain and the handgrip muscles in six adult patients with leprosy presenting the claw hand deformity. As expected, handgrip was generally weaker in the patients’ more affected hands relative to the less affected hands and to those of healthy individuals. Also, two out of the four tested hand muscles had a relatively smaller representation in the brain if compared to other muscles in the same patient or in healthy individuals. Interestingly, the ulnar nerve, which makes the connection between the brain and the two muscles with smaller representation, was more affected by the disease than other nerves in the same patient. On the other hand, a muscle connected to the brain by a nerve less affected showed stronger neuroelectrical signal, indicating a more robust evoked response. This finding demonstrates that the brain representation for a given muscle may change depending on the degree of damage in the nerve connecting the muscle to the brain, which is evidence for brain plasticity.
“Our findings indicate that the cortical motor area corresponding to the most affected hand suffers changes, revealing that that the damage caused by leprosy is not limited to peripheral nerve injury”, says Dr. Vargas.
A better understanding of the relationship between limb dysfunction caused by leprosy and brain plasticity may help develop new treatment strategies for the millions of individuals currently suffering from this ancient disease.
Funding: This study was supported by the National Counsel of Technological and Scientific Development, Carlos Chagas Filho Foundation for Research Support in the State of Rio de Janeiro, Brazilian Innovation Agency, and others.
Source: Claudia Vargas – PUBLICASE COMUNICAÇÃO CIENTÍFICA
Image Credit: The image is credited to Vargas et al./PLOS Neglected Tropical Diseases.
Original Research: Full open access research for “Primary Motor Cortex Representation of Handgrip Muscles in Patients with Leprosy” by Vagner Wilian Batista e Sá, Maria Katia Gomes, Maria Luíza Sales Rangel, Tiago Arruda Sanchez, Filipe Azaline Moreira, Sebastian Hoefle, Inaiacy Bittencourt Souto, Antônio José Ledo Alves da Cunha, Ana Paula Fontana, and Claudia Domingues Vargas in PLOS Neglected Tropical Diseases. Published online July 23 2015 doi:10.1371/journal.pntd.0003944
Abstract
Primary Motor Cortex Representation of Handgrip Muscles in Patients with Leprosy
Background
Leprosy is an endemic infectious disease caused by Mycobacterium leprae that predominantly attacks the skin and peripheral nerves, leading to progressive impairment of motor, sensory and autonomic function. Little is known about how this peripheral neuropathy affects corticospinal excitability of handgrip muscles. Our purpose was to explore the motor cortex organization after progressive peripheral nerve injury and upper-limb dysfunction induced by leprosy using noninvasive transcranial magnetic stimulation (TMS).
Methods
In a cross-sectional study design, we mapped bilaterally in the primary motor cortex (M1) the representations of the hand flexor digitorum superficialis (FDS), as well as of the intrinsic hand muscles abductor pollicis brevis (APB), first dorsal interosseous (FDI) and abductor digiti minimi (ADM). All participants underwent clinical assessment, handgrip dynamometry and motor and sensory nerve conduction exams 30 days before mapping. Wilcoxon signed rank and Mann-Whitney tests were performed with an alpha-value of p<0.05.
Findings
Dynamometry performance of the patients’ most affected hand (MAH), was worse than that of the less affected hand (LAH) and of healthy controls participants (p = 0.031), confirming handgrip impairment. Motor threshold (MT) of the FDS muscle was higher in both hemispheres in patients as compared to controls, and lower in the hemisphere contralateral to the MAH when compared to that of the LAH. Moreover, motor evoked potential (MEP) amplitudes collected in the FDS of the MAH were higher in comparison to those of controls. Strikingly, MEPs in the intrinsic hand muscle FDI had lower amplitudes in the hemisphere contralateral to MAH as compared to those of the LAH and the control group. Taken together, these results are suggestive of a more robust representation of an extrinsic hand flexor and impaired intrinsic hand muscle function in the hemisphere contralateral to the MAH due to leprosy.
Conclusion
Decreased sensory-motor function induced by leprosy affects handgrip muscle representation in M1.
“Primary Motor Cortex Representation of Handgrip Muscles in Patients with Leprosy” by Vagner Wilian Batista e Sá, Maria Katia Gomes, Maria Luíza Sales Rangel, Tiago Arruda Sanchez, Filipe Azaline Moreira, Sebastian Hoefle, Inaiacy Bittencourt Souto, Antônio José Ledo Alves da Cunha, Ana Paula Fontana, and Claudia Domingues Vargas in PLOS Neglected Tropical Diseases. Published online July 23 2015 doi:10.1371/journal.pntd.0003944






