Summary: Glioblastoma can mimic the normal repair of white matter in the brain, causing the tumor to become less malignant. Additionally, a drug commonly prescribed for asthma can help suppress glioblastoma growth in mouse models.
Source: UCL
Scientists at the UCL have made a ‘surprising’ discovery that glioblastoma, an aggressive brain cancer, mimics normal brain repair in white matter, which leads to the tumor becoming less malignant.
In the study on mice, funded by Cancer Research UK and published in Nature Communications, researchers used these novel findings to identify drugs which could be used, or repurposed, to harness this response (feature) and treat the cancer.
Using the pre-clinical mouse models, the researchers found that Pranlukast, a drug clinically approved for treating asthma in people, suppressed glioblastoma growth.
Explaining the research, lead author, Professor Simona Parrinello (UCL Cancer Institute),said:“We know glioblastoma often develops and spreads in the brain’s white matter but it has been unclear why this happens or what molecules are involved in this process.
“In this experimental study, we wanted to understand what impact white matter has on cancerous tumour cells.”
Glioblastomas are the most aggressive type of cancer that begins within the brain. One of the main reasons that glioblastomas are so difficult to treat is that they spread into different regions of the brain. Approximately half the brain is grey matter, made up of cell bodies including neurons, the other half, referred to as white matter is composed of neuronal projections which are insulated by fatty membranes and therefore appear white. Tumor cells use the white matter as a route to spread to other brain regions.
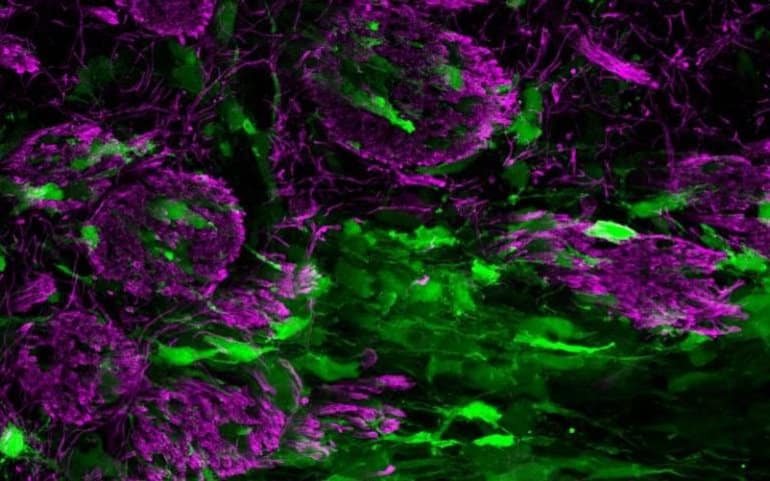
In this study, the research team discovered that tumour cells, mimic brain repair, in that they attempt to repair the damage that the growing tumour mass causes to the brain’s white matter.
Professor Parrinello, who is Group Leader at the Samantha Dickson Brain Cancer Unit, part of UCL Cancer Institute, explained: “To our surprise, when the tumor cells spread into the brain’s white matter, it made the glioblastoma less aggressive.
“This response is caused by the growing tumor injuring the white matter and in turn responding to this wound-like environment by attempting to repair it.
“This causes the tumor cells to mature into cells that resemble the normal brain cells that make up the white matter.
“In this mature state, tumor cells become less able to grow and spread.”
The team found that this tumor response can be exploited for glioblastoma treatment using drugs that promote normal white matter repair, such as Pranlukast.
Professor Parrinello added: “Glioblastoma is the most common and aggressive type of primary brain tumour. There are currently no effective treatments for glioblastoma, so recurrence is inevitable. As a result, prognosis for glioblastoma patients remains extremely poor with a median survival of less than 18 months. Here we identified a potential new approach to treat glioblastoma and show that a drug currently in clinical use for asthma suppresses glioblastoma growth and spread in preclinical models.”
Around 2,200 people in the UK (mostly adults) are diagnosed with glioblastoma each year and currently prognosis is extremely poor with average survival rate of around six to 18 months.
Michelle Mitchell, chief executive of Cancer Research UK, said: “Brain tumours are notoriously hard to treat because we still don’t know enough about the biology of the disease, and current treatments are not effective enough. This early research is fascinating as it could mean an existing asthma drug may help people with glioblastoma. Repurposing a drug that has already passed safety tests would save a lot of time compared to developing a new treatment from scratch, time which would make an incredible difference to the lives of people affected by glioblastoma.”
About this brain cancer research news
Source: UCL
Contact: Henry Killworth – UCL
Image: The image is credited to Lucy Brooks
Original Research: Open access.
“The white matter is a pro-differentiative niche for glioblastoma” by Lucy J. Brooks, Melanie P. Clements, Jemima J. Burden, Daniela Kocher, Luca Richards, Sara Castro Devesa, Leila Zakka, Megan Woodberry, Michael Ellis, Zane Jaunmuktane, Sebastian Brandner, Gillian Morrison, Steven M. Pollard, Peter B. Dirks, Samuel Marguerat & Simona Parrinello. Nature Communications
Abstract
The white matter is a pro-differentiative niche for glioblastoma
Glioblastomas are hierarchically organised tumours driven by glioma stem cells that retain partial differentiation potential. Glioma stem cells are maintained in specialised microenvironments, but whether, or how, they undergo lineage progression outside of these niches remains unclear.
Here we identify the white matter as a differentiative niche for glioblastomas with oligodendrocyte lineage competency. Tumour cells in contact with white matter acquire pre-oligodendrocyte fate, resulting in decreased proliferation and invasion.
Differentiation is a response to white matter injury, which is caused by tumour infiltration itself in a tumoursuppressive feedback loop. Mechanistically, tumour cell differentiation is driven by selective white matter upregulation of SOX10, a master regulator of normal oligodendrogenesis.
SOX10 overexpression or treatment with myelination-promoting agents that upregulate endogenous SOX10, mimic this response, leading to niche-independent pre-oligodendrocyte differentiation and tumour suppression in vivo.
Thus, glioblastoma recapitulates an injury response and exploiting this latent programme may offer treatment opportunities for a subset of patients.