Summary: Using human-induced pluripotent stem cells, researchers have identified a gene signaling pathway linked to a higher risk of developing schizophrenia.
Source: UT Health
Using human-induced pluripotent stem cells engineered from a single family’s blood samples, a gene signaling pathway linked to a higher risk for developing schizophrenia was discovered by scientists at The University of Texas Health Science Center at Houston (UTHealth). The research was published in a recent issue of Neuropsychopharmacology.
The signaling pathway researchers pinpointed is called phosphoinositide 3-kinase/glycogen synthase kinase 3 (PI3K/GSK3). Among the differentially expressed genes along the pathway was one called serum-glucocorticoid kinase 1 (SGK1), an inhibitor of GSK3 beta, which has been associated with schizophrenia.
“We believe this has direct implications for the treatment of patients,” said senior author Consuelo Walss-Bass, PhD, professor in the Louis A. Faillace, MD, Department of Psychiatry and Behavioral Sciences at McGovern Medical School at UTHealth. “There is a new antipsychotic that just received approval from the Food and Drug Administration that directly targets the pathway we identified as dysregulated in neurons from the patients, and several other antipsychotics also target this pathway. This could help pinpoint who may respond better to treatments.”
Researchers led by Walss-Bass and first author, postdoctoral research fellow Laura Stertz, PhD, used blood samples from adult members of a large family with multiple individuals affected by schizophrenia. Through human-induced pluripotent stem cell (hiPSC) technology, the blood cells were reprogrammed into stem cells, which were then directed to become brain neurons.
Those neurons could be studied in a virtual biopsy and compared to neurons engineered from individuals who did not have schizophrenia, but came from the same family from a homogenous population in the Central Valley of Costa Rica.
“Mental health research has lagged behind because we don’t know what is happening biologically. We are diagnosing people based on what they are telling us,” Walss-Bass said. “Even postmortem, the brain tissue in mental health disorders looks perfectly fine. In Alzheimer’s disease, you can see a difference compared to controls. But not in psychiatric disorders. Now by studying virtual brain biopsies, we can tell what is happening biologically.”
Among the differentially expressed genes the researchers saw in the virtual biopsies were five that have previously been identified as schizophrenia candidate genes by genome-wide association studies.
Among the genes associated with the PI3K/GSK3 pathway was SGK1, which inhibits GSK3 activity. Those alterations are linked to whether a person has a higher risk of developing schizophrenia.
“We were able to find significant, meaningful differences with a small control group,” Walss-Bass said. “Neurons of patients with schizophrenia had alterations in the signaling pathway. This research may help to understand how or why some antipsychotics targeting GSK3 work and also to develop other target-specific medications.”
Walss-Bass said identifying patients with specific biological pathway markers could identify them as the best candidates for medications, creating the personal pharmacology that is needed to treat psychiatric disorders.
Funding: The study was supported by an award from The University of Texas System (UT BRAIN), and a Brain and Behavior Research Foundation Young Investigator Award to Stertz.
UTHealth co-authors were Gabriel R. Fries, PhD; Emily Mendez; Laura Smith Callahan, PhD; Ying Liu, PhD; and Zhongming Zhao, PhD. Fries is an assistant professor in the Faillace Department of Psychiatry and Behavioral Sciences. Smith Callahan and Liu are assistant and associate professor, respectively, in the Vivian L. Smith Department of Neurosurgery at McGovern Medical School. Zhou is a professor with UTHealth School of Biomedical Informatics and UTHealth School of Public Health. Walss-Bass, Fries, Liu, and Smith Callahan are members, and Mendez is an MD/PhD student, with The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences.
About this genetics and schizophrenia research news
Source: UT Health
Contact: Deborah Mann Lake – UT Health
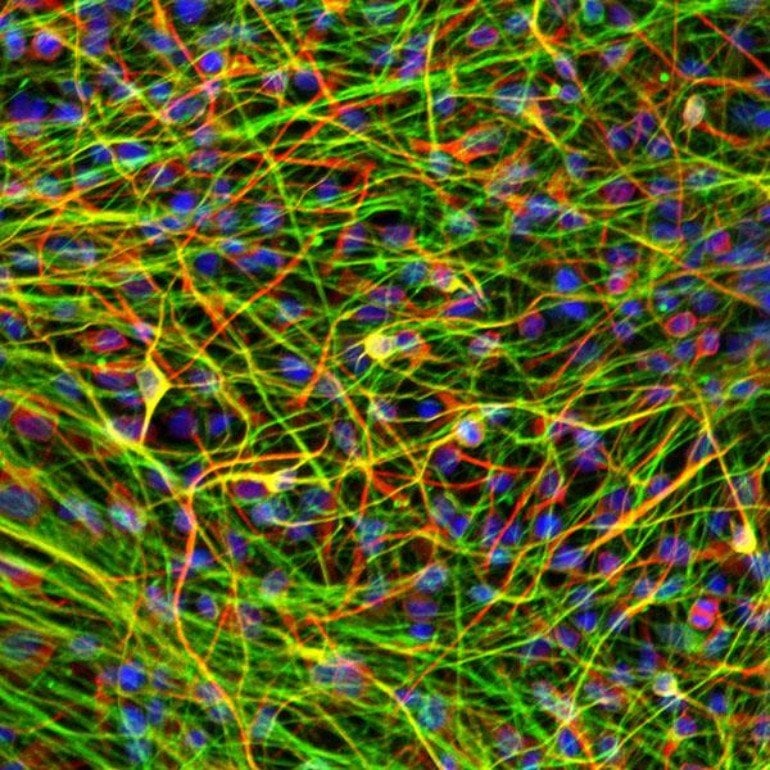
Image: The image is credited to Laura Stertz, PhD/UTHealth
Original Research: Closed access.
“Convergent genomic and pharmacological evidence of PI3K/GSK3 signaling alterations in neurons from schizophrenia patients” by Laura Stertz, Jessica Di Re, Guangsheng Pei, Gabriel R. Fries, Emily Mendez, Shenglan Li, Laura Smith-Callahan, Henriette Raventos, Jerricho Tipo, Rohan Cherukuru, Zhongming Zhao, Ying Liu, Peilin Jia, Fernanda Laezza & Consuelo Walss-Bas. Neuropsychopharmacology
Abstract
Convergent genomic and pharmacological evidence of PI3K/GSK3 signaling alterations in neurons from schizophrenia patients
Human-induced pluripotent stem cells (hiPSCs) allow for the establishment of brain cellular models of psychiatric disorders that account for a patient’s genetic background. Here, we conducted an RNA-sequencing profiling study of hiPSC-derived cell lines from schizophrenia (SCZ) subjects, most of which are from a multiplex family, from the population isolate of the Central Valley of Costa Rica. hiPSCs, neural precursor cells, and cortical neurons derived from six healthy controls and seven SCZ subjects were generated using standard methodology. Transcriptome from these cells was obtained using Illumina HiSeq 2500, and differential expression analyses were performed using DESeq2 (|fold change|>1.5 and false discovery rate < 0.3), in patients compared to controls. We identified 454 differentially expressed genes in hiPSC-derived neurons, enriched in pathways including phosphoinositide 3-kinase/glycogen synthase kinase 3 (PI3K/GSK3) signaling, with serum-glucocorticoid kinase 1 (SGK1), an inhibitor of glycogen synthase kinase 3β, as part of this pathway. We further found that pharmacological inhibition of downstream effectors of the PI3K/GSK3 pathway, SGK1 and GSK3, induced alterations in levels of neurite markers βIII tubulin and fibroblast growth factor 12, with differential effects in patients compared to controls. While demonstrating the utility of hiPSCs derived from multiplex families to identify significant cell-specific gene network alterations in SCZ, these studies support a role for disruption of PI3K/GSK3 signaling as a risk factor for SCZ.






