Summary: A new study reveals that a brain circuit driving negative emotions during cocaine withdrawal plays a key role in relapse. Researchers found that this “anti-reward” network becomes hyperactive during abstinence, amplifying distress and pushing users back toward the drug.
Paradoxically, this circuit may also serve as a protective brake by making drug use emotionally costly. The findings offer a fresh perspective on addiction treatment by targeting withdrawal-related pain, not just craving.
Key Facts:
- Anti-Reward Circuit: A brain network amplifies emotional distress during withdrawal.
- Relapse Trigger: Heightened negative feelings drive users back to cocaine.
- Protective Role: The same circuit may help limit excessive drug use.
Source: Hebrew University of Jerusalem
Why do so many people relapse after quitting cocaine?
A new study from The Hebrew University reveals that a specific “anti-reward” brain circuit becomes hyperactive during withdrawal—driving discomfort and pushing users back toward the drug.
Surprisingly, this circuit may also serve as a built-in protective mechanism, offering new hope for addiction treatment.

Cocaine addiction has long been understood as a tug-of-war between reward and restraint. The rush of dopamine keeps users hooked, while withdrawal triggers anxiety, depression, and despair.
But a new study by researchers at The Hebrew University of Jerusalem reveals that it’s not just the craving for pleasure—but the brain’s aversion to pain—that plays a powerful role in relapse.
Led by Prof. Yonatan M. Kupchik and PhD student Liran Levi from the Faculty of Medicine, the study identifies a specific “anti-reward” network deep in the brain that undergoes lasting changes during cocaine use, withdrawal, and re-exposure.
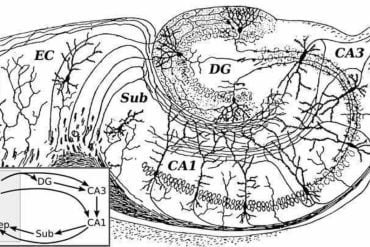
This glutamatergic network, located in the ventral pallidum, is emerging as a key player in addiction—and a promising target for future therapies.
The rollercoaster inside the brain
While the ventral pallidum is known for regulating pleasure and reward, this research highlights a lesser-known group of neurons that suppress dopamine release and amplify negative emotions.
During abstinence, this anti-reward network ramps up its activity—intensifying discomfort and emotional distress. When cocaine is reintroduced, the network quickly quiets, reinforcing the cycle of relief-seeking and relapse.
“It’s a switch,” says Prof. Kupchik. “This network tracks the emotional cost of abstinence. When it’s highly active, it can drive someone to seek out the drug again—just to escape the negative feelings.”
The study also shows that this brain circuit connects with other key centers involved in emotional regulation and reward processing. During withdrawal, these connections become stronger, increasing sensitivity to negative emotional states. When the drug returns, the system resets—temporarily easing distress.
Surprisingly, discomfort may serve a purpose
In a striking finding, the researchers discovered that when this anti-reward circuit was inhibited, drug preference and motivation actually increased. This suggests that the brain’s negative signals may serve a protective role—creating an internal brake that discourages excessive drug use by making it emotionally costly.
A shift in the addiction treatment paradigm
While most current addiction therapies aim to dampen the brain’s reward system, this study points to a different path: targeting the emotional pain of withdrawal. By understanding and potentially modulating the brain’s aversive signals, future treatments may better address the root causes of relapse.
Published by PhD student Liran A. Levi and Prof. Kupchik at Hebrew University’s IMRIC Center for Addiction Research (ICARe), the study offers a new framework for understanding addiction—not just as the pursuit of pleasure, but as the escape from pain.
About this addiction and mental health research news
Author: Danae Marx
Source: Hebrew University of Jerusalem
Contact: Danae Marx – Hebrew University of Jerusalem
Image: The image is credited to Neuroscience News
Original Research: Open access.
“A ventral pallidal glutamatergic aversive network encodes abstinence from and re-exposure to cocaine” by Liran A. Levi et al. Science Advances
Abstract
A ventral pallidal glutamatergic aversive network encodes abstinence from and re-exposure to cocaine
Relapse to drugs of abuse can occur after long periods of abstinence. The ventral pallidum (VP) is central to drug addiction, and its glutamatergic neurons (VPGlu), whose activation drives aversion, inhibit drug seeking.
However, it remains unknown whether these neurons encode the abstinence from and relapse to drugs.
We show here that VPGlu projections specifically to the aversion-related lateral habenula (LHb) and ventral tegmental area gabaergic (VTAGABA) neurons show plasticity induced by abstinence from and reexposure to cocaine or cocaine cues.
Both these pathways potentiate during abstinence and restore baseline values upon drug reexposure but with different plasticity mechanisms.
Last, inhibiting the VPGlu → LHb pathway enhances cocaine preference after abstinence, while inhibiting the VPGlu → VTA pathway shows variable effects.
These findings establish an aversive circuit orchestrated by VPGlu neurons encoding long-term abstinence-driven changes that may contribute to drug relapse.