Summary: Study reveals how the brain’s opioid system is linked to mood changes associated with depression and anxiety. Neuroimaging revealed, in those with depression, there is a decreased number of opioid receptors in specific areas of the brain.
Source: University of Turku
A new study conducted in Turku, Finland, reveals how symptoms indicating depression and anxiety are linked to brain function changes already in healthy individuals.
Researchers of the national Turku PET Centre have shown that the opioid system in the brain is connected to mood changes associated with depression and anxiety.
Depression and anxiety are typically associated with lowered mood and decreased experience of pleasure. Opioids regulate the feelings of pain and pleasure in the brain. The new study conducted in Turku shows that the symptoms associated with depression and anxiety are connected to changes in the brain’s opioid system already in healthy individuals.
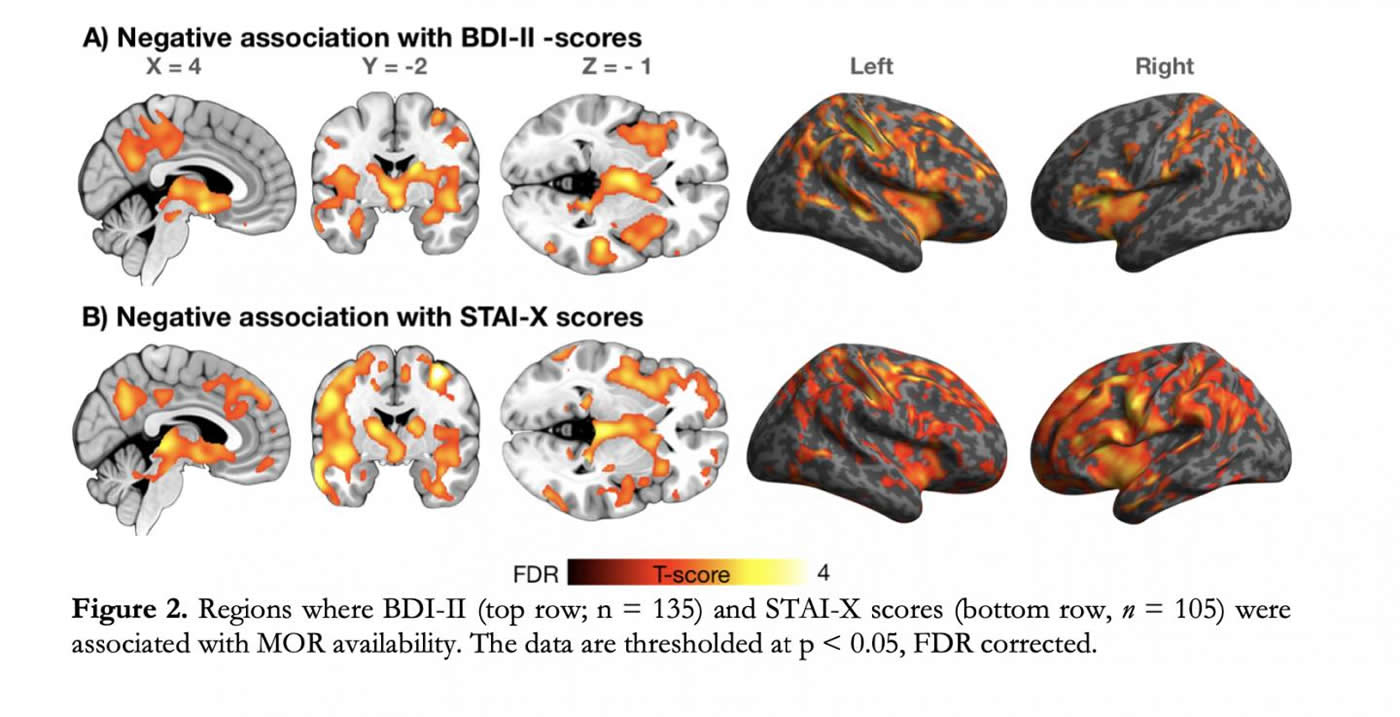
“We found that the more depressive and anxious symptoms the subjects had, the less opioid receptors there were in their brain. These receptors function like small “docks” that are influenced by both the brains own opioids as well as opiates. These type of opioid-mediated mood changes can be an important mechanism in the central nervous system,” says Professor Lauri Nummenmaa from the University of Turku.
“These results show that the mood changes indicating depression can be detected in the brain already early on. Both the brain’s own opioids and synthetic opiate-based drugs regulate mood. Based on the results, drugs that have an effect on the opioid system can help in the treatment of depression,” adds Nummenmaa.
The study was conducted with Positron Emission Tomography (PET) and altogether 135 volunteers participated as subjects. A small dose of radioactive tracer binding to the brain’s opioid receptors was injected in their circulation. The decay of the tracers was measured with a PET camera, whereas the depressive and anxious symptoms of the subjects were measured with questionnaires.
The study is based on the AIVO database hosted by Turku University Hospital and Turku PET Centre. The database contains different in vivo molecular brain scans for extensive analyses: https://aivo.utu.fi/
The results have been published in the Neuropsychopharmacology journal.
Funding: The study was funded by the Academy of Finland and Sigrid Jusélius Foundation.
About this neuroscience research article
Source:
University of Turku
Media Contacts:
Lauri Nummenmaa – University of Turku
Image Source:
The image is credited to Lauri Nummenmaa.
Original Research: Closed access
“Lowered endogenous mu-opioid receptor availability in subclinical depression and anxiety”. by Lauri Nummenmaa, Tomi Karjalainen, Janne Isojärvi, Tatu Kantonen, Jouni Tuisku, Valtteri Kaasinen, Juho Joutsa, Pirjo Nuutila, Kari Kalliokoski, Jussi Hirvonen, Jarmo Hietala & Juha Rinne.
Neuropsychopharmacology doi:10.1038/s41386-020-0725-9
Abstract
Lowered endogenous mu-opioid receptor availability in subclinical depression and anxiety
Major depressive disorder is associated with lowered mood, anxiety, anhedonia, sleep problems, and cognitive impairments. Many of these functions are regulated by μ-opioid receptor (MOR) system. Preclinical, in vivo, and post-mortem studies have however yielded inconclusive results regarding the role of the MOR in depression and anxiety. Moreover, it is not known whether alterations in MOR are already present in subclinical depression and anxiety. In a large-scale retrospective cross-sectional study we pooled data from 135 (113 males and 22 females) healthy subjects whose brain’s MOR availability was measured with positron emission tomography (PET) using an agonist radioligand [11C]carfentanil that has high affinity for MORs. Depressive and anxious symptomology was addressed with BDI-II and STAI-X questionnaires, respectively. Both anxiety and depression scores in the subclinical range were negatively associated with MOR availability in cortical and subcortical areas, notably in amygdala, hippocampus, ventral striatum, and orbitofrontal and cingulate cortices. We conclude that dysregulated MOR availability is involved in altered mood and pathophysiology of depression and anxiety disorders.






