A study of 35 families led by a UC San Francisco psychiatric researcher showed for the first time that the structure of the brain circuitry known as the corticolimbic system is more likely to be passed down from mothers to daughters than from mothers to sons or from fathers to children of either gender.
The corticolimbic system governs emotional regulation and processing and plays a role in mood disorders, including depression.
A large body of human clinical research indicates a strong association in depression between mothers and daughters, while many previous animal studies have shown that female offspring are more likely than males to show changes in emotion-associated brain structures in response to maternal prenatal stress. Until now, however, there have been few studies that attempted to link the two streams of research, said lead author Fumiko Hoeft, MD, PhD, a UCSF associate professor of psychiatry.
The finding does not mean that mothers are necessarily responsible for their daughters’ depression, Hoeft said. “Many factors play a role in depression – genes that are not inherited from the mother, social environment and life experiences, to name only three. Mother-daughter transmission is just one piece of it.
“But this is the first study to bridge animal and human clinical research and show a possible matrilineal transmission of human corticolimbic circuitry, which has been implicated in depression, by scanning both parents and offspring,” said Hoeft, who directs the UCSF Hoeft Laboratory for Educational Neuroscience. “It opens the door to a whole new avenue of research looking at intergenerational transmission patterns in the human brain.”
The study was published in the Journal of Neuroscience on Jan. 27.
Brain Structures in Healthy Families
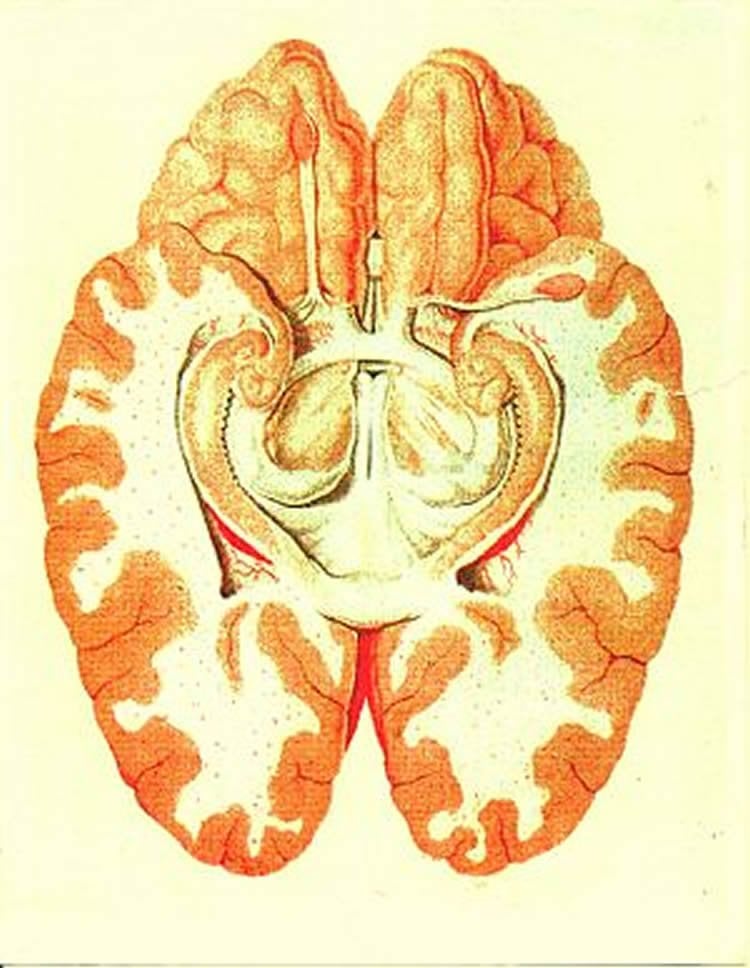
The corticolimbic system includes the amygdala, hippocampus, anterior cingulate cortex and ventromedial prefrontal cortex. Hoeft and her research team used non-invasive magnetic resonance imaging (MRI) to measure grey matter volume (GMV) in the corticolimbic systems of parents and their biological offspring from 35 healthy families. None of the family members were diagnosed with depression. The association between mothers’ and daughters’ corticolimbic GMV was significantly greater than that between mothers and sons, fathers and sons, and fathers and daughters.
The study is the first to use MRI in both parents and their children to study intergenerational transmission of the pattern of brain structures, said Hoeft. “This gives us a potential new tool to better understand depression and other neuropsychiatric conditions, as most conditions seem to show intergenerational transmission patterns,” she said. “Anxiety, autism, addition, schizophrenia, dyslexia, you name it – brain patterns inherited from both mothers and fathers have an impact on just about all of them.”
Studying Maternal Influence in IVF
One limitation of the study, said Hoeft, is that it does not differentiate between the potential effects of genetics, prenatal conditions and postnatal conditions on the inheritance of brain structures. She hopes that a new study funded by the UCSF Academic Senate, which is just getting under way, will address that shortcoming.
Hoeft and her team will use MRI to study brain structures in families where children have been conceived and delivered using different types of in vitro fertilization (IVF).
The researchers will image the brains of parents and children in families where the birth mother was implanted with a donor egg; families where a surrogate was implanted with the biological mother’s egg; and families where the mother was implanted with her own fertilized egg in a procedure known as homologous IVF.
“With donor eggs, there is no maternal genetic input, but there is maternal prenatal and postnatal influence,” Hoeft explained. “In gestational surrogacy, there is genetic and postnatal input from the biological mother, but no prenatal input. With homologous IVF, there are maternal genetic, prenatal and postnatal influences. Comparison of these three groups allows us to control for potential effects of the IVF procedure itself.”
By studying these different family groups, she said, “we will for the very first time be able to examine, and hopefully distinguish between, the effects of genetics, prenatal environment and postnatal environment on brain function, structure, and cognitive function.”
While Hoeft and her team are funded to look at corticolimbic circuitry, “this does not preclude our looking at other brain systems,” she said. “We will be examining the language network, the reward system and different networks implicated in psychosis. We will cast a wide net, gain a lot of information and maximize this fantastic opportunity.”
Other authors of the current study are Roeland Hancock, PhD, and Tony Yang, MD, PhD, of UCSF; Bun Yamagata, MD, PhD, and Masaru Mimura, MD, PhD, of Keio University School of Medicine, Tokyo, Japan; Kou Murayama, PhD, of the University of Reading, Reading, UK; Jessica Black, PhD, of Boston College; and Allan Reiss, MD, of Stanford University.
Funding: The study was supported by funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute of Mental Health, the National Science Foundation, the UCSF Dyslexia Center, a UCSF Academic Senate award, a UCSF-CCC Neuroscience Fellowship and the Dennis & Shannon Wong – DSEA ’88 Foundation.
Source: Steve Tokar – UCSF
Image Source: The image is in the public domain
Original Research: The research will appear in Journal of Neuroscience during the week of January 25 2016.






