Summary: New research shows that individuals with cannabis use disorder have elevated dopamine levels in brain regions associated with psychosis. Using neuromelanin-sensitive MRI scans, scientists found increased dopamine activity, visible as darker brain spots, in cannabis users regardless of schizophrenia diagnosis.
These changes suggest accelerated dopamine-related aging in the brain, helping explain the rise in cannabis-induced psychosis seen clinically since legalization. The findings highlight the need for greater public awareness about cannabis use and its potential mental health risks.
Key Facts:
- Dopamine Spike: Cannabis use disorder is linked to increased dopamine in brain regions associated with psychosis.
- Imaging Evidence: Neuromelanin-sensitive MRI revealed darker brain spots indicating excess dopamine in cannabis users.
- Public Health Concern: Findings may explain the rise in cannabis-related psychosis and underscore the need for informed cannabis use education.
Source: Western University
Although it’s been six years since cannabis was legalized in Canada, further research is needed to fully understand its health effects.
A new study published April 9 in JAMA Psychiatry sheds light on how cannabis use disorder is linked to changes in the brain that are associated with psychosis.

Using brain imaging techniques, researchers found individuals with cannabis use disorder, those who were using cannabis on a frequent basis over an extended period of time, exhibited signs of higher levels of dopamine in the same region of the brain that is tied to psychosis.
This study was conducted in London, Ont., led by researchers from London Health Sciences Centre Research Institute (LHSCRI) and Western’s Schulich School of Medicine & Dentistry.
Previous data has shown that in emergency departments across Canada, people have been presenting more often with psychosis after the legalization of cannabis.
“We now have evidence that shows a straight line linking cannabis with dopamine and psychosis that has never been shown before, and it’s crucial that clinicians, patients, and families work together to break this line,” said Lena Palaniyappan, adjunct professor at Schulich Medicine & Dentistry, former medical director for LHSC’s Prevention and Early Intervention Program for Psychosis (PEPP) and the senior author of the study.
Dopamine is an important neurotransmitter (a chemical messenger in the brain) that helps process motivation, mood, learning and motor control.
“Excess levels of dopamine can disrupt normal brain processes and may increase the risk of psychosis, particularly in individuals who are already vulnerable,” said Betsy Schaefer, co-author of the study at LHSCRI and study coordinator at PEPP.
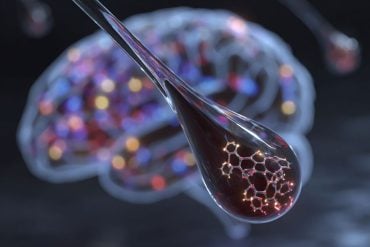
Using a non-invasive brain imaging technique called neuromelanin-sensitive magnetic resonance imaging, researchers were able to look at a substance called neuromelanin – a black pigment left behind in the brain that accumulates over time if there is too much dopamine.
The neuromelanin appears in the scans as black spots, acting as a marker to measure and identify areas with dopamine activity.
“In people partaking in excess cannabis use, those spots are blacker than what they should be for their age compared to healthy individuals.
This indicates they have high levels of dopamine, and in some cases are showing pigments someone 10 years older would have,” said Palaniyappan, who is also a professor at McGill University.
Sixty-one participants aged 18- to 35-years-old were involved in this study. Researchers recruited individuals with and without cannabis use disorder, with some in each group also diagnosed with first-episode schizophrenia, who presented to PEPP at LHSC.
“We saw an increase of blacker spots in a particular region of the midbrain associated with psychosis –the substantia nigra and ventral tegmental areas.
“This increase was seen in those with cannabis use disorder regardless of whether they have first-episode schizophrenia,” said Ali Khan, Schulich Medicine & Dentistry professor and scientist at Robarts Research Institute.
“This research really helps to provide evidence, or the smoking gun, of what we’re seeing clinically and provides clues as to why exposure to cannabis is causing brain changes linked to psychosis.” – Dr. Julie Richard, psychiatrist and physician lead of PEPP at LHSC
“In the last several years since legalization, we’re seeing adolescents who have two or three brief cannabis-induced episodes of psychosis and then have a much more major episode.
“So, we’re trying to counsel adolescents within that first episode that they’re pushing their brain towards a major episode and show them the areas in the brain that are impacted,” said Richard.
Shaefer explained the new research helps clarify the biological mechanisms connecting cannabis use and mental health risks. The findings underscore the need for awareness, especially as cannabis becomes more widely used since legalization.
“We hope this study encourages further research and informs public health policies to support safe and informed cannabis use.”
“I hope these findings lead patients and health-care providers to better understand the implications and for the health-care providers to give patients resources for options other than cannabis to help them cope,” said first author Jessica Ahrens, PhD candidate at McGill University.
About this cannabis use disorder and psychosis research news
Author: Cynthia Fazio
Source: Western University
Contact: Cynthia Fazio – Western University
Image: The image is credited to Neuroscience News
Original Research: Closed access.
“Convergence of Cannabis and Psychosis on the Dopamine System” by Lena Palaniyappan et al. JAMA Psychiatry
Abstract
Convergence of Cannabis and Psychosis on the Dopamine System
Importance
Despite evidence that individuals with a cannabis use disorder (CUD) are at elevated risk of psychosis and that the neurotransmitter dopamine has a role in psychosis, the mechanism linking cannabis use and psychosis remains unclear.
Objective
To use neuromelanin-sensitive magnetic resonance imaging (MRI), referred to as the neuromelanin-MRI signal, a practical, proxy measure of dopamine function, to assess whether a common alteration in the dopamine system may be implicated in CUD and psychosis and whether this alteration can be observed in those with a CUD whether or not they have a diagnosis of first-episode schizophrenia (FES).
Design, Setting, and Participants
This longitudinal observational cohort study recruited individuals from 2019 to 2023 from an early psychosis service and the surrounding communities in London, Ontario. The sample included individuals with and without CUD, with some in each group also diagnosed with FES.
Exposures
FES and CUD diagnoses from the Structured Clinical Interview for DSM-5.
Main Outcomes and Measures
Neuromelanin-MRI signals within the midbrain (substantia nigra [SN]/ventral tegmental area [VTA]) including a subregion previously linked to the severity of untreated psychosis (a priori region of interest). Linear mixed-effects analyses were performed relating neuromelanin-MRI signals to clinical measures.
Results
A total of 36 individuals without CUD (mean [SD] age, 22.3 [3.2] years; 29 male [81%]; 12 with FES) and 25 individuals with CUD (mean [SD] age, 24.3 [4.7] years; 22 male [88%]; 16 with FES) participated in the study.
One-year follow-up was completed for 12 individuals with CUD and 25 without CUD. CUD was associated with elevated neuromelanin-MRI signal in a set of ventral SN/VTA voxels (387 of 2060 SN/VTA voxels, corrected P = .03, permutation test).
CUD was also associated with elevated neuromelanin-MRI signal in the psychosis-related region of interest (t92 = 2.12, P = .04) with a significant dose-dependent association (higher burden of CUD symptoms associated with higher neuromelanin-MRI signal, F1, 96 = 4.89; P = .03).
In contrast, participants with FES did not exhibit a significant elevation in neuromelanin-MRI signal (241 SN/VTA voxels had elevated signal, corrected P = .09). There was no association between time and neuromelanin-MRI signal.
Conclusions and Relevance
Elevated dopamine function in a critical SN/VTA subregion may be associated with psychosis risk in people with CUD. Cannabis was associated with the hypothesized final common pathway for the clinical expression of psychotic symptoms.