Summary: Calcium signaling was found to be a central abnormality in schizophrenia neurons. Targeting calcium signaling in neurons could be a potential new way to treat the 16p11.2 duplication variation of schizophrenia.
Source: Northwestern University
Targeting calcium signaling in neurons represents a promising therapeutic approach for treating a rare form of schizophrenia, according to a Northwestern Medicine study published in Biological Psychiatry.
“This is the first time that human neurons are made and characterized from schizophrenia patients with the 16p11.2 duplication, one of the most prominent genetic risk factors in schizophrenia, and the first time that calcium signaling is found as a central abnormality in schizophrenia neurons,” said Peter Penzes, Ph.D., the Ruth and Evelyn Dunbar Professor of Psychiatry and Behavioral Sciences and senior author of the study.
Schizophrenia is characterized by auditory and visual hallucinations, delusions, and trouble with forming and sorting thoughts, which severely impacts productivity and overall quality of life. The disease, which affects roughly one percent of the general population, has strong genetic associations, however the exact genes involved are unknown.
Patients with schizophrenia can be treated with antipsychotics, however those drugs only address “positive symptoms,” such as hallucinations and delusions, and neglect to treat cognitive symptoms such as thought disorder. Despite the availability of antipsychotics, only some patients will respond to them and the development of new treatments has been met with challenges, according to Penzes.
“This has been hampered by the fact that studies in animal models, such as mice, do not translate well to humans. In other words, some new drugs may work well in experimental animal studies, but fail when taken into human clinical trials,” said Penzes, who is also a professor of Neuroscience, of Pharmacology and director of the Center for Autism and Neurodevelopment.
A potential solution to developing new therapies for schizophrenia is induced pluripotent stem cells (iPSCs), cells derived from a patient’s blood or skin that can be reprogrammed to be any type of cell in the body, including neurons.
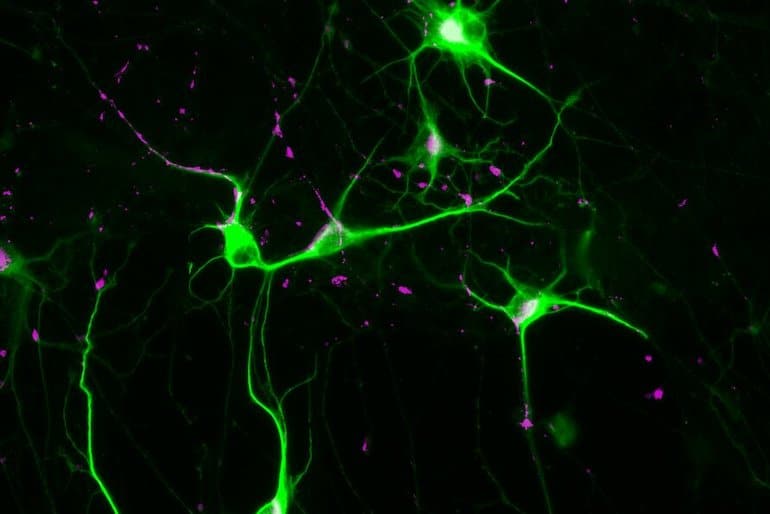
In the current study, the investigators created iSPC-derived neurons from two patients with a rare form of schizophrenia containing the “16p11.2 duplication” mutation, which increases the risk of developing schizophrenia by sixteenfold, and three healthy patients. Neuronal cell lines were grown in Penzes’ laboratory for seven weeks until complete neuronal networks were formed.
Using multiple advanced techniques including calcium imaging microscopy, high throughput electrophysiology and RNA sequencing, the investigators found that calcium signaling—when neurons communicate using calcium ions to promote cellular signaling and other essential intracellular functions—functions abnormally in the brain cells of patients with schizophrenia when compared to healthy neurons.
According to Penzes, next steps will involve using these iSPC-derived neurons to screen for novel drugs to treat this genetic form of schizophrenia. If successful, the drugs may be useful to treat patients with schizophrenia in general and other neurological disorders.
“The 16p11.2 mutation is also a prominent risk factor for autism; hence such drugs could also then be tested for treating autism,” Penzes said.
About this schizophrenia research news
Author: Melissa Rohman
Source: Northwestern University
Contact: Melissa Rohman – Northwestern University
Image: The image is credited to Euan Parnell, PhD
Original Research: Open access.
“Excitatory Dysfunction Drives Network and Calcium Handling Deficits in 16p11.2 Duplication Schizophrenia Induced Pluripotent Stem Cell–Derived Neurons” by Euan Parnell et al. Biological Psychiatry
Abstract
Excitatory Dysfunction Drives Network and Calcium Handling Deficits in 16p11.2 Duplication Schizophrenia Induced Pluripotent Stem Cell–Derived Neurons
Background
Schizophrenia (SCZ) is a debilitating psychiatric disorder with a large genetic contribution; however, its neurodevelopmental substrates remain largely unknown. Modeling pathogenic processes in SCZ using human induced pluripotent stem cell–derived neurons (iNs) has emerged as a promising strategy. Copy number variants confer high genetic risk for SCZ, with duplication of the 16p11.2 locus increasing the risk 14.5-fold.
Methods
To dissect the contribution of induced excitatory neurons (iENs) versus GABAergic (gamma-aminobutyric acidergic) neurons (iGNs) to SCZ pathophysiology, we induced iNs from CRISPR (clustered regularly interspaced short palindromic repeats)-Cas9 isogenic and SCZ patient–derived induced pluripotent stem cells and analyzed SCZ-related phenotypes in iEN monocultures and iEN/iGN cocultures.
Results
In iEN/iGN cocultures, neuronal firing and synchrony were reduced at later, but not earlier, stages of in vitro development. These were fully recapitulated in iEN monocultures, indicating a primary role for iENs. Moreover, isogenic iENs showed reduced dendrite length and deficits in calcium handling. iENs from 16p11.2 duplication-carrying patients with SCZ displayed overlapping deficits in network synchrony, dendrite outgrowth, and calcium handling. Transcriptomic analysis of both iEN cohorts revealed molecular markers of disease related to the glutamatergic synapse, neuroarchitecture, and calcium regulation.
Conclusions
Our results indicate the presence of 16p11.2 duplication-dependent alterations in SCZ patient–derived iENs. Transcriptomics and cellular phenotyping reveal overlap between isogenic and patient-derived iENs, suggesting a central role of glutamatergic, morphological, and calcium dysregulation in 16p11.2 duplication-mediated pathogenesis. Moreover, excitatory dysfunction during early neurodevelopment is implicated as the basis of SCZ pathogenesis in 16p11.2 duplication carriers. Our results support network synchrony and calcium handling as outcomes directly linked to this genetic risk variant.






