Summary: According to a new study, children and young adults with chronic kidney disease have changes in cerebral blood flow that could increase the risk of cognitive impairment.
Source: RSNA.
Blood flow changes in the brains of children, adolescents and young adults with chronic kidney disease may explain why many face a higher risk of cognitive impairment, according to a study published online in the journal Radiology.
Prior research has linked chronic kidney disease, a condition characterized by the loss of kidney function over time, with lesions in the brain’s signal-carrying white matter and deficits in cognitive performance. While chronic kidney disease in adults is frequently associated with age-related disorders such as hypertension and diabetes, the disease in childhood often occurs congenitally, yet still affects brain development and cognitive function.
“It’s not clear if the brain problems from kidney disease seen in adults are secondary to the hypertension produced by the disease,” said coauthor John A. Detre, M.D., professor of neurology and radiology, director of the Center for Functional Neuroimaging in Radiology and vice chair for research in neurology at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia. “In our study, we wanted to look at patients with early kidney disease, before they’ve experienced decades of high blood pressure. In doing this, we could separate the kidney disease effects from those of chronic high blood pressure.”
Dr. Detre and colleagues assessed blood flow in the brains of 73 pediatric kidney disease patients, average age just under 16 years, and 57 similarly aged control participants. The researchers used arterial spin labeling, an MRI technique that can noninvasively quantify blood flow in the brain.
Patients with kidney disease showed higher cerebral blood flow compared with controls in certain brain regions — a surprising finding, considering that decreased cognitive performance is generally associated with decreased blood flow in the brain, such as in aging and dementia. There are a couple of possible reasons for this unusual phenomenon, Dr. Detre said.
“It may indicate compensatory hyperactivity, in which the brain regions are working extra hard to maintain performance,” he said. “Another possibility is that there’s a disturbance in the regulation of blood flow in these patients.”
White matter cerebral blood flow and blood pressure were also correlated, suggesting that kidney disease patients have problems with cerebrovascular autoregulation, the process that controls blood pressure in the brain. This type of dysfunction could potentially lead to white matter injury, according to Dr. Detre.
“Chronic kidney disease appears to affect brain physiology and function even early in the disease,” he said. “This study gives us clues about what changes in brain physiology might underlie cognitive changes.”
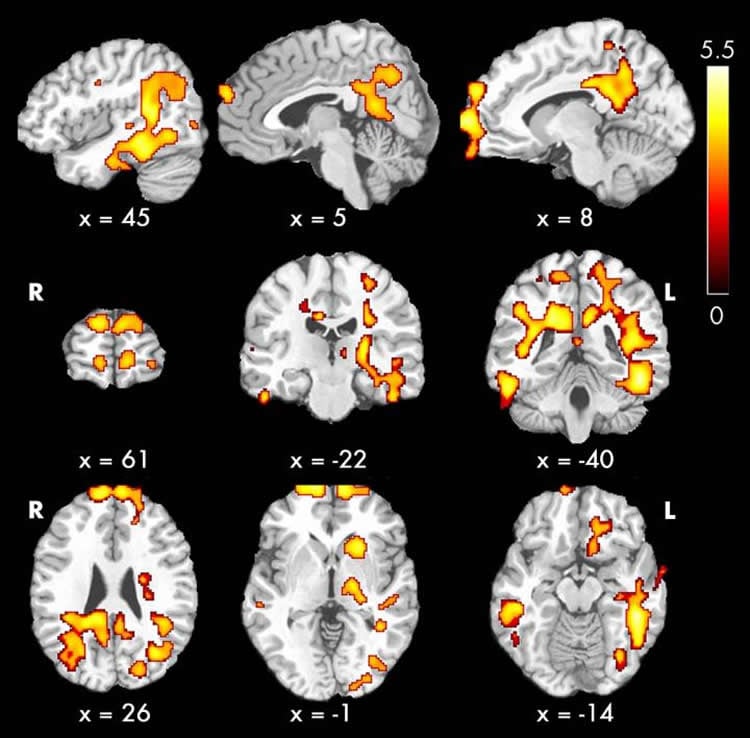
Among those changes were differences in blood flow between patients and controls in areas of the brain that correlated with cognitive problems in the patients. Compared with controls, kidney disease patients had cerebral blood flow differences in the default-mode network, the network of brain regions active when a person is not focused on a particular task. Patients with low executive function, or skills related to planning, organizing and paying attention, had significant differences in cerebral blood flow compared with controls.
The findings point to cerebral blood flow measurements with arterial spin labeling as a potentially valuable tool in characterizing cerebrovascular function in chronic kidney disease — an important area of research given the associations between kidney disease and neurological function, and the significantly increased risk for transient ischemic attack and stroke in even mild chronic kidney patients.
“Cerebral blood flow is a critically important physiological parameter that you can measure in just a few minutes with arterial spin labeling,” Dr. Detre said. “This technique provides a noninvasive way of quantifying cerebral blood flow that doesn’t require use of contrast agent, which is contraindicated in patients with kidney dysfunction.”
Funding: This project is supported by a Commonwealth Universal Research Enhancement grant with the Pennsylvania Department of Health.
Source: Linda Brooks – RSNA
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is credited to RSNA.
Original Research: Abstract for “Regional Cerebral Blood Flow in Children and Young Adults with Chronic Kidney Disease” by Hua-Shan Liu, Erum A. Hartung, Abbas F. Jawad, Jeffrey B. Ware, Nina Laney, Allison M. Port, Ruben C. Gur, Stephen R. Hooper, Jerilynn Radcliffe, Susan L. Furth, and John A. Detre in Radiology. Published June 12 2018
doi:10.1148/radiol.2018171339
[cbtabs][cbtab title=”MLA”]RSNA “Children with Kidney Disease Show Blood Flow Changes in Brain.” NeuroscienceNews. NeuroscienceNews, 12 June 2018.
<https://neurosciencenews.com/brain-blood-flow-kidney-disease-9320/>.[/cbtab][cbtab title=”APA”]RSNA (2018, June 12). Children with Kidney Disease Show Blood Flow Changes in Brain. NeuroscienceNews. Retrieved June 12, 2018 from https://neurosciencenews.com/brain-blood-flow-kidney-disease-9320/[/cbtab][cbtab title=”Chicago”]RSNA “Children with Kidney Disease Show Blood Flow Changes in Brain.” https://neurosciencenews.com/brain-blood-flow-kidney-disease-9320/ (accessed June 12, 2018).[/cbtab][/cbtabs]
Abstract
Regional Cerebral Blood Flow in Children and Young Adults with Chronic Kidney Disease
Purpose
To investigate the pathophysiologic effects of chronic kidney disease (CKD) on brain function in children with CKD by correlating cerebral blood flow (CBF) with clinical and behavioral indexes.
Materials and Methods
In this prospective study, 73 pediatric patients with CKD (mean age, 15.80 years ± 3.63; range, 9–25 years) and 57 control subjects (mean age, 15.65 years ± 3.76; range, 9–25 years) were recruited. CBF measurements were acquired with an MRI arterial spin labeling scheme. Neurocognitive measurements were performed with traditional and computerized neurocognitive batteries. Clinical data were also collected. Group-level global and regional CBF differences between patients with CKD and control subjects were assessed. Regression analyses were conducted to evaluate the associations among regional CBF, clinical variables, and cognitive performance.
Results
Patients with CKD showed higher global CBF compared with control subjects that was attributable to reduced hematocrit level (mean, 60.2 mL/100 g/min ± 9.0 vs 56.5 mL/100 g/min ± 8.0, respectively). White matter CBF showed correlation with blood pressure (r = 0.244, P = .039), a finding suggestive of altered cerebrovascular autoregulation. Regional CBF differences between patients and control subjects included regions in the “default mode” network. In patients with CKD, positive extrema in the precuneus showed a strong correlation with executive function (ρ = 0.608, P = .001).
Conclusion
Systemic effects of estimated glomerular filtration rate, hematocrit level, and blood pressure on CBF and alterations in regional CBF may reflect impaired brain function underlying neurocognitive symptoms in CKD. These findings further characterize the nature of alterations in brain physiologic features in children, adolescents, and young adults with CKD.