Summary: Researchers report exosomes help neuron-to-neuron growth and the transfer of oligomer amyloid beta, resulting in apoptosis. The study reveals exosomes may be a primary mediator of the pathogenic progression of Alzheimer’s disease.
Source: Springer.
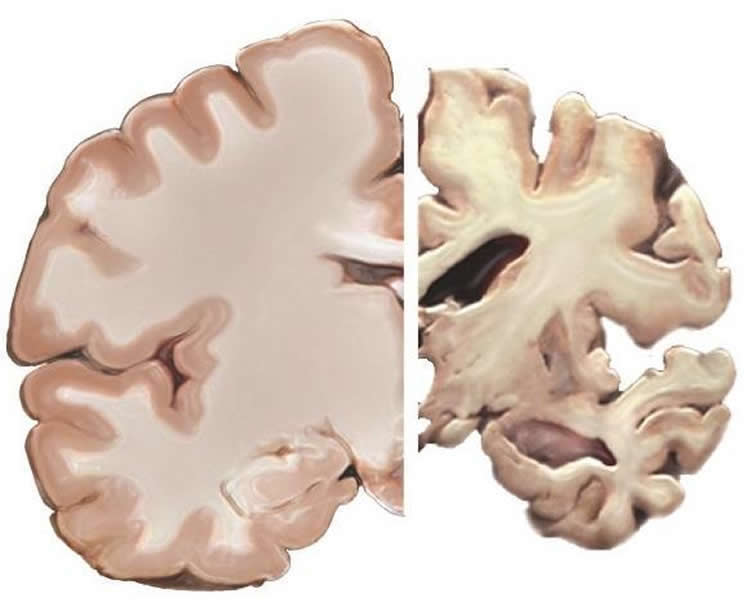
Scientists have pinpointed minute exosomes as the main vehicle that allow the spread of toxic proteins that trigger the onset of Alzheimer’s Disease across a person’s brain network. This finding could help to develop better diagnostic and treatment options for this debilitating brain disease that is characterized by dementia, memory loss, mood swings and being disorientated and is ultimately fatal. The research is published in Springer’s journal Acta Neuropathologica, with Maitrayee Sardar Sinha and Anna Ansell-Schultz of Linköping University in Sweden as lead researchers.
Previous studies have linked the development of Alzheimer’s to the gradual and abnormal build-up in the brain of two toxic types of amino acids, amyloid-beta (Aβ) and tau. The Swedish group, led by Martin Hallbeck, involved in this study had also previously shown how oligomer amoloid-beta (an intermediate product of amyloid-beta) accumulates inside cells and subsequently spreads from one cell to another.
In this study, the team focused on exosomes to better understand how such proteins build up and spread across the brain and therefore increase the effects of Alzheimer’s Disease over time. Exosomes are vesicles or fluid-filled sacs found outside of cells. They are extremely small and only range from 20 to 120 nanometers in diameter – at best the size of a virus. Exosomes play a role in cellular communication and the transport of different types of molecules in both healthy and diseased bodies.
The researchers compared the post mortem brain samples of ten people (five of whom had lived with Alzheimer’s) obtained from the brain bank at Uppsala University in Sweden. Various microscopy and cell-characterizing cytometric techniques were used in the process.
The exosomes isolated from Alzheimer’s patients were found to contain greater concentrations of toxic oligomer amyloid-beta compared to healthy brains. A definite link between intracellular oligomer amyloid-beta and extracellular exosomes was also found, in that these were co-localized and occurred together. The researchers established that exosomes help neuron-to-neuron growth and transfer of oligomer amyloid-beta, which in turn could cause brain cells to die. Exosomes carrying oligomer amyloid-beta were internalized in cultured neurons and were able to spread their toxic content to nearby cells. Some of the exosomes were found to be transferred intact to further cells. This finding is consistent with a recent study showing that a substantial fraction of exosomes internalized in one cell was subsequently passed on to a second cell.
“Exosomes could be the main mediator of the pathogenic progression in Alzheimer’s Disease, and might therefore be exploited to develop new diagnostic and therapeutic principles related to the disease,” Sardar Sinha explains.
Because of their small size, neuronal exosomes are released into reasonably accessible body fluids such as blood and cerebrospinal fluid, which can be drawn to measure the level of oligomer amoloid-beta build up in a person’s body.
“Hence, measurement of increased oligomer amoloid-beta in exosomes from such patient samples could potentially serve as a diagnostic tool,” says Ansell-Schultz, who describes the molecular content of exosomes as a “fingerprint” of the releasing cell type.
Source: Elizabeth Hawkins – Springer
Publisher: Organized by NeuroscienceNews.com.
Image Source: NeuroscienceNews.com image is in the public domain.
Original Research: Open access research for “Alzheimer’s disease pathology propagation by exosomes containing toxic amyloid-beta oligomers” by Maitrayee Sardar Sinha, Anna Ansell-Schultz, Livia Civitelli, Camilla Hildesjö, Max Larsson, Lars Lannfelt, Martin Ingelsson, and Martin Hallbeck in Acta Neuropathologica. Published June 13 2018.
doi:10.1007/s00401-018-1868-1
[cbtabs][cbtab title=”MLA”]Springer “Insights Into Amyloids Associated with Alzheimer’s and Type 2 Diabetes.” NeuroscienceNews. NeuroscienceNews, 28 June 2018.
<https://neurosciencenews.com/alzheimers-spread-9468/>.[/cbtab][cbtab title=”APA”]Springer (2018, June 28). Insights Into Amyloids Associated with Alzheimer’s and Type 2 Diabetes. NeuroscienceNews. Retrieved June 28, 2018 from https://neurosciencenews.com/alzheimers-spread-9468/[/cbtab][cbtab title=”Chicago”]Springer “Insights Into Amyloids Associated with Alzheimer’s and Type 2 Diabetes.” https://neurosciencenews.com/alzheimers-spread-9468/ (accessed June 28, 2018).[/cbtab][/cbtabs]
Abstract
Alzheimer’s disease pathology propagation by exosomes containing toxic amyloid-beta oligomers
The gradual deterioration of cognitive functions in Alzheimer’s disease is paralleled by a hierarchical progression of amyloid-beta and tau brain pathology. Recent findings indicate that toxic oligomers of amyloid-beta may cause propagation of pathology in a prion-like manner, although the underlying mechanisms are incompletely understood. Here we show that small extracellular vesicles, exosomes, from Alzheimer patients’ brains contain increased levels of amyloid-beta oligomers and can act as vehicles for the neuron-to-neuron transfer of such toxic species in recipient neurons in culture. Moreover, blocking the formation, secretion or uptake of exosomes was found to reduce both the spread of oligomers and the related toxicity. Taken together, our results imply that exosomes are centrally involved in Alzheimer’s disease and that they could serve as targets for development of new diagnostic and therapeutic principles.






