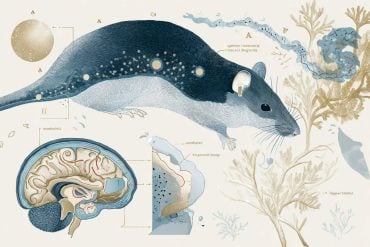
Summary: A diet containing compounds found in green tea and carrots reversed Alzheimer’s-like symptoms in mice genetically programmed to develop symptoms of the disease, USC researchers say.
Source: University of Southern California
Researchers emphasize that the study, published in the Journal of Biological Chemistry, was in mice, and many mouse discoveries never translate into human treatments. Nevertheless, the findings lend credence to the idea that certain readily available, plant-based supplements might offer protection against dementia in humans.
“You don’t have to wait 10 to 12 years for a designer drug to make it to market; you can make these dietary changes today,” said senior author Terrence Town, a professor of physiology and neuroscience at the Keck School of Medicine of USC’s Zilkha Neurogenetic Institute. “I find that very encouraging.”
Diet and Alzheimer’s: Combination therapy
What’s more, the study supports the idea that combination therapy, rather than a single magic bullet, may offer the best approach to treating the 5.7 million Americans living with Alzheimer’s. Combination treatment is already the standard of care for diseases such as cancer, HIV infection and rheumatoid arthritis.
For this study, the researchers took a look at two compounds, EGCG, or epigallocatechin-3-gallate, a key ingredient in green tea, and FA, or ferulic acid, which is found in carrots, tomatoes, rice, wheat and oats.
The researchers randomly assigned 32 mice with Alzheimer’s-like symptoms to one of four groups with an equal number of males and females. For comparison, each group also included an equal number of healthy mice. For three months, the mice consumed a combination of EGCG and FA, or EGCG or FA only, or a placebo. The dosage was 30 milligrams per kilogram of body weight — a dosage well-tolerated by humans and easily consumed as part of a healthy diet.
Diet and Alzheimer’s: Testing results
Before and after the three-month special diet, scientists ran the mice through a battery of neuropsychological tests that are roughly analogous to the thinking and memory tests that assess dementia in humans. Of particular note was a maze in the shape of a Y, which tests a mouse’s spatial working memory — a skill that humans use to find their way out of a building.
Healthy mice instinctively explore each arm of the Y maze, looking for food or a route to escape and entering the three arms in sequence more often than by chance alone. Impaired mice can’t do this as well as their mentally healthy counterparts.
“After three months, combination treatment completely restored spatial working memory and the Alzheimer’s mice performed just as well as the healthy comparison mice,” Town said.
How did it work? Town says one mechanism appeared to be the substances’ ability to prevent amyloid precursor proteins from breaking up into the smaller proteins called amyloid beta that gum up Alzheimer patients’ brains. In addition, the compounds appeared to reduce neuroinflammation and oxidative stress in the brain—key aspects of Alzheimer’s pathology in humans.
Town said he and his lab will continue exploring combination treatment, with a focus on plant-derived substances that inhibit production of the sticky amyloid beta plaques.
Source: University of Southern California
By: Leigh Hopper – USC
Original Research: Abstract for “Combined treatment with the phenolics (−)-epigallocatechin-3-gallate and ferulic acid improves cognition and reduces Alzheimer-like pathology in mice” in Journal of Biological Chemistry. February 22, 2019
doi: 10.1074/jbc.RA118.004280
Funding: The study was supported by grants from the National Institutes of Health (2R01NS076794-06A1, 1RF1AG053982-01A1, 5P01AG052350-03 and 5R21AG053884-02), the Japan Society for the Promotion of Science (KAKENHI JP26430058), an Alzheimer’s Association Sex and Gender in Alzheimer’s disease grant, Cure Alzheimer’s Fund, and the Rotary Coins for Alzheimer’s Research Trust.
Abstract
Combined treatment with the phenolics (−)-epigallocatechin-3-gallate and ferulic acid improves cognition and reduces Alzheimer-like pathology in mice
“Nutraceuticals” are well-tolerated natural dietary compounds with drug-like properties that make them attractive as Alzheimer’s disease (AD) therapeutics. Combination therapy for AD has garnered attention following a recent National Institute on Aging mandate, but this approach has not yet been fully validated. In this report, we combined the two most promising nutraceuticals with complementary anti-amyloidogenic properties: the plant-derived phenolics (−)-epigallocatechin-3-gallate (EGCG, an α-secretase activator) and ferulic acid (FA, a β-secretase modulator). We used transgenic mice expressing mutant human amyloid β-protein precursor and presenilin 1 (APP/PS1) to model cerebral amyloidosis. At 12 months of age, we orally administered EGCG and/or FA (30 mg/kg each) or vehicle once daily for 3 months. At 15 months, combined EGCG–FA treatment reversed cognitive impairment in most tests of learning and memory, including novel object recognition and maze tasks. Moreover, EGCG- and FA-treated APP/PS1 mice exhibited amelioration of brain parenchymal and cerebral vascular β-amyloid deposits and decreased abundance of amyloid β-proteins compared with either EGCG or FA single treatment. Combined treatment elevated nonamyloidogenic soluble APP-α and α-secretase candidate and down-regulated amyloidogenic soluble APP-β, β-C-terminal APP fragment, and β-secretase protein expression, providing evidence for a shift toward nonamyloidogenic APP processing. Additional beneficial co-treatment effects included amelioration of neuroinflammation, oxidative stress, and synaptotoxicity. Our findings offer preclinical evidence that combined treatment with EGCG and FA is a promising AD therapeutic approach.