New analysis links cognitive, emotional, and intellectual symptoms to neurological ‘disruption’ in multiple brain regions – a finding with important implications for diagnosis and treatment.
Schizophrenia, a severe mental disorder affecting about one in 100 people, is notoriously difficult to diagnose and treat, in large part because it manifests differently in different people. A new study published today in Molecular Neuropsychiatry helps explain why. Researchers at the University of North Carolina School of Medicine have created a map that shows how specific schizophrenia symptoms are linked to distinct brain circuits.
The findings add to a growing body of evidence that schizophrenia is not a single disease but a complex constellation of neural circuit problems. The study also reinforces the potential value of brain scans for identifying and understanding schizophrenia in individual patients, for finding promising new therapeutic approaches, and for helping clinicians track a patient’s progress during therapy.
“For a long time, we’ve thought of brain imaging studies as mainly a way to corroborate or confirm aspects of brain function and pathology that we had already identified from studying a patient’s behavior,” said Aysenil Belger, PhD, professor of psychiatry and psychology at UNC and the study’s senior author. “This approach, where we use brain imaging to dissect the specific neural pathways of complex syndromes, is very novel and important. The imaging can help us distinguish between the different brain networks that contribute to distinct sub-symptoms. These distinctions are not recognizable from behavioral observations alone.”
Belger, the director of the UNC Neurocognition and Imaging Research Laboratory, and recent UNC graduate student Joseph Shaffer, PhD, compared brain scans from more than 100 people with schizophrenia against brain scans from people with no psychiatric diagnoses. The scans were acquired as part of a large multi-site national collaborative research project, the Biomedical Informatics Research Network. Researchers imaged participants during a non-invasive test in which subjects were asked to listen to simple tones and detect changes in pitch.
The analysis revealed that people with schizophrenia showed markedly less brain activity during detection of the tonal changes as compared to the control group, a difference that became more apparent as symptoms worsened.
The study’s most novel and striking findings emerged when researchers analyzed patterns of brain activity in patients with different types of schizophrenia symptoms. They focused on schizophrenia’s so-called “negative” symptoms, such as problems with speech, blunted emotions, lack of motivation, and an inability to experience pleasure. (“Positive” symptoms include delusions, thought disorders, and hallucinations.) Negative symptoms are the hardest to treat with available medications and can make it difficult to hold a job or form relationships.
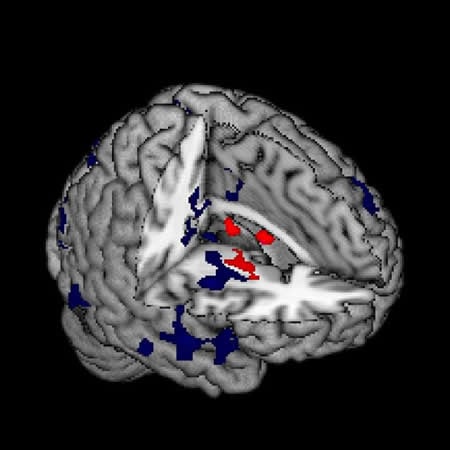
A close analysis of the brain scans revealed vastly different neural circuitry behind problems that seem similar on the surface. While a clinician may find it difficult to parse whether a patient’s stilted conversational manner is rooted in a lack of emotional connection or problems forming words, a brain scan in Belger’s study made it clear, for example, that particular symptoms were more closely associated with disruption in the brain’s emotional processing areas, whereas other symptoms were more closely associated with regions responsible for language and motor control.
“We were surprised by the degree to which these circuits were connected with different sub-symptoms, and by what was, in some cases, almost a complete lack of circuit overlap between these different sub-symptoms,” said Belger.
Parsing these complex symptoms could help inform new treatment approaches for schizophrenia and other disorders. “Many of these sub-symptoms are seen in other neuropsychiatric disorders, as well. Therefore, finding the neurological pathway or developing a treatment for that specific symptom could help to address multiple disorders,” Belger said.
Also, the findings could help improve the tools available for early detection of risk for schizophrenia and psychosis, which are typically not diagnosed until late adolescence. If clinicians could use brain scans to identify vulnerable high-risk individuals in early adolescence when the brain is still developing, it may be possible to curb the development of the disorder and help prevent its most debilitating effects. Belger also indicated that such “high-risk” mapping studies are currently being conducted at the University of North Carolina in collaboration with Diana Perkins, MD, and collaborators at multiple institutions across the country under the North American Prodrome Longitudinal Study (NAPLS).
Brain scans used in the study were acquired from the Function Biomedical Informatics Research Network, a National Institutes of Health-funded network to facilitate data sharing and online collaboration among researchers. Study co-authors include Joseph Shaffer, Michael Peterson and Joshua Bizzell of UNC; Mary Agnes McMahon and Jim Voyvodic of the Duke-UNC Brain Imaging and Analysis Center; Vince Calhoun of the Mind Research Network and the University of New Mexico; Theo van Erp and Adrian Preda of the University of California, Irvine; Judith Ford, Daniel Mathalon and Steven Potkin of the University of California, San Francisco; John Lauriello of the University of Missouri; Kelvin Lim of the University of Minnesota, Minneapolis; Dara Manoach of Massachusetts General Hospital; Sarah McEwen of the University of California, Los Angeles; Daniel O’Leary of the University of Iowa; Jessica Turner of Georgia State University; and Cynthia Wible of Harvard Medical School and VA Medical Center Brockton.
Funding: This work received support from the NIH.
Source: Mark Derewicz – University of North Carolina School of Medicine
Image Credit: The image is credited to UNC School of Medicine
Original Research: Full open access research for “Neural Correlates of Schizophrenia Negative Symptoms: Distinct Subtypes Impact Dissociable Brain Circuits” by Shaffer J.J., Peterson M.J., McMahon M.A., Bizzell J., Calhoun V., van Erp T.G.M., Ford J.M., Lauriello J., Lim K.O., Manoach D.S., McEwen S.C., Mathalon D.H., O’Leary D., Potkin S.G., Preda A., Turner J., Voyvodic J., Wible C.G., and Belger A. in Molecular Neuropsychiatry. Published online November 2015 doi:10.1159/000440979
Abstract
Neural Correlates of Schizophrenia Negative Symptoms: Distinct Subtypes Impact Dissociable Brain Circuits
Background: The negative symptoms of schizophrenia include deficits in emotional expression and motivation. These deficits are stable over the course of illness and respond poorly to current medications. Previous studies have focused on negative symptoms as a single category; however, individual symptoms might be related to separate neurological disturbances. We analyzed data from the Functional Biomedical Informatics Research Network dataset to explore the relationship between individual negative symptoms and functional brain activity during an auditory oddball task.
Methods: Functional magnetic resonance imaging was conducted on 89 schizophrenia patients and 106 healthy controls during a two-tone auditory oddball task. Blood oxygenation level-dependent (BOLD) signal during the target tone was correlated with severity of five negative symptom domains from the Scale for the Assessment of Negative Symptoms.
Results: The severity of alogia, avolition/apathy and anhedonia/asociality was negatively correlated with BOLD activity in distinct sets of brain regions associated with processing of the target tone, including basal ganglia, thalamus, insular cortex, prefrontal cortex, posterior cingulate and parietal cortex.
Conclusions: Individual symptoms were related to different patterns of functional activation during the oddball task, suggesting that individual symptoms might arise from distinct neural mechanisms. This work has potential to inform interventions that target these symptom-related neural disruptions.
“Neural Correlates of Schizophrenia Negative Symptoms: Distinct Subtypes Impact Dissociable Brain Circuits” by Shaffer J.J., Peterson M.J., McMahon M.A., Bizzell J., Calhoun V., van Erp T.G.M., Ford J.M., Lauriello J., Lim K.O., Manoach D.S., McEwen S.C., Mathalon D.H., O’Leary D., Potkin S.G., Preda A., Turner J., Voyvodic J., Wible C.G., and Belger A. in Molecular Neuropsychiatry. Published online November 2015 doi:10.1159/000440979