Summary: A new neuroprosthetic interface allows prosthetic limbs to be controlled by the body’s nervous system, resulting in a natural walking gait. The surgery reconnects muscles, providing proprioceptive feedback, enabling users to walk faster and navigate obstacles more effectively.
The study compared patients with this interface to those with traditional prosthetics, finding significant improvements in movement and coordination. This breakthrough offers promising advancements in prosthetic technology and patient care.
Key Facts:
- The new neuroprosthetic interface reconnects muscles, enhancing natural control.
- Patients with this interface walk faster and more naturally than those with traditional prosthetics.
- The study’s findings may lead to improved prosthetic technologies and patient outcomes.
Source: MIT
State-of-the-art prosthetic limbs can help people with amputations achieve a natural walking gait, but they don’t give the user full neural control over the limb. Instead, they rely on robotic sensors and controllers that move the limb using predefined gait algorithms.
Using a new type of surgical intervention and neuroprosthetic interface, MIT researchers, in collaboration with colleagues from Brigham and Women’s Hospital, have shown that a natural walking gait is achievable using a prosthetic leg fully driven by the body’s own nervous system.
The surgical amputation procedure reconnects muscles in the residual limb, which allows patients to receive “proprioceptive” feedback about where their prosthetic limb is in space.
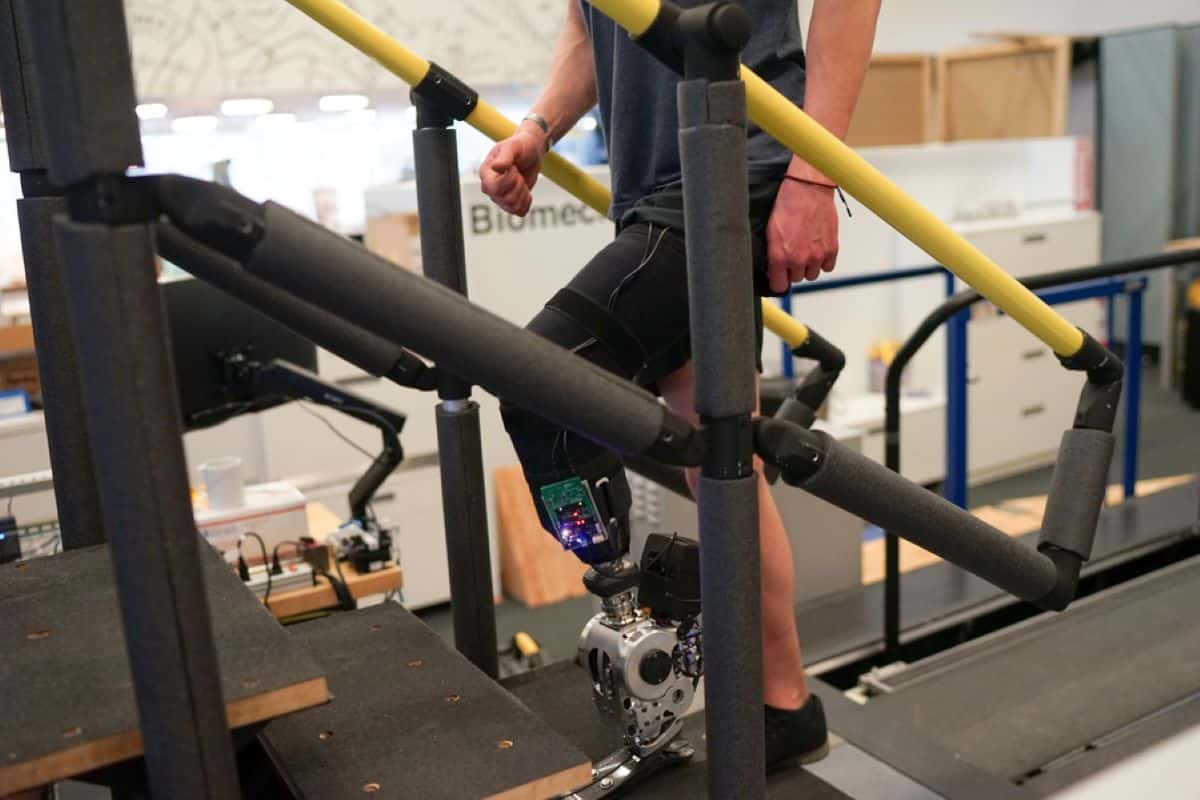
In a study of seven patients who had this surgery, the MIT team found that they were able to walk faster, avoid obstacles, and climb stairs much more naturally than people with a traditional amputation.
“This is the first prosthetic study in history that shows a leg prosthesis under full neural modulation, where a biomimetic gait emerges. No one has been able to show this level of brain control that produces a natural gait, where the human’s nervous system is controlling the movement, not a robotic control algorithm,” says Hugh Herr, a professor of media arts and sciences, co-director of the K. Lisa Yang Center for Bionics at MIT, an associate member of MIT’s McGovern Institute for Brain Research, and the senior author of the new study.
Patients also experienced less pain and less muscle atrophy following this surgery, which is known as the agonist-antagonist myoneural interface (AMI). So far, about 60 patients around the world have received this type of surgery, which can also be done for people with arm amputations.
Hyungeun Song, a postdoc in MIT’s Media Lab, is the lead author of the paper, which appears today in Nature Medicine.
Sensory feedback
Most limb movement is controlled by pairs of muscles that take turns stretching and contracting. During a traditional below-the-knee amputation, the interactions of these paired muscles are disrupted. This makes it very difficult for the nervous system to sense the position of a muscle and how fast it’s contracting — sensory information that is critical for the brain to decide how to move the limb.
People with this kind of amputation may have trouble controlling their prosthetic limb because they can’t accurately sense where the limb is in space. Instead, they rely on robotic controllers built into the prosthetic limb. These limbs also include sensors that can detect and adjust to slopes and obstacles.
To try to help people achieve a natural gait under full nervous system control, Herr and his colleagues began developing the AMI surgery several years ago. Instead of severing natural agonist-antagonist muscle interactions, they connect the two ends of the muscles so that they still dynamically communicate with each other within the residual limb.
This surgery can be done during a primary amputation, or the muscles can be reconnected after the initial amputation as part of a revision procedure.
“With the AMI amputation procedure, to the greatest extent possible, we attempt to connect native agonists to native antagonists in a physiological way so that after amputation, a person can move their full phantom limb with physiologic levels of proprioception and range of movement,” Herr says.
In a 2021 study, Herr’s lab found that patients who had this surgery were able to more precisely control the muscles of their amputated limb, and that those muscles produced electrical signals similar to those from their intact limb.
After those encouraging results, the researchers set out to explore whether those electrical signals could generate commands for a prosthetic limb and at the same time give the user feedback about the limb’s position in space. The person wearing the prosthetic limb could then use that proprioceptive feedback to volitionally adjust their gait as needed.
In the new Nature Medicine study, the MIT team found this sensory feedback did indeed translate into a smooth, near-natural ability to walk and navigate obstacles.
“Because of the AMI neuroprosthetic interface, we were able to boost that neural signaling, preserving as much as we could. This was able to restore a person’s neural capability to continuously and directly control the full gait, across different walking speeds, stairs, slopes, even going over obstacles,” Song says.
A natural gait
For this study, the researchers compared seven people who had the AMI surgery with seven who had traditional below-the-knee amputations. All of the subjects used the same type of bionic limb: a prosthesis with a powered ankle as well as electrodes that can sense electromyography (EMG) signals from the tibialis anterior the gastrocnemius muscles. These signals are fed into a robotic controller that helps the prosthesis calculate how much to bend the ankle, how much torque to apply, or how much power to deliver.
The researchers tested the subjects in several different situations: level-ground walking across a 10-meter pathway, walking up a slope, walking down a ramp, walking up and down stairs, and walking on a level surface while avoiding obstacles.
In all of these tasks, the people with the AMI neuroprosthetic interface were able to walk faster — at about the same rate as people without amputations — and navigate around obstacles more easily.
They also showed more natural movements, such as pointing the toes of the prosthesis upward while going up stairs or stepping over an obstacle, and they were better able to coordinate the movements of their prosthetic limb and their intact limb. They were also able to push off the ground with the same amount of force as someone without an amputation.
“With the AMI cohort, we saw natural biomimetic behaviors emerge,” Herr says. “The cohort that didn’t have the AMI, they were able to walk, but the prosthetic movements weren’t natural, and their movements were generally slower.”
These natural behaviors emerged even though the amount of sensory feedback provided by the AMI was less than 20 percent of what would normally be received in people without an amputation.
“One of the main findings here is that a small increase in neural feedback from your amputated limb can restore significant bionic neural controllability, to a point where you allow people to directly neurally control the speed of walking, adapt to different terrain, and avoid obstacles,” Song says.
“This work represents yet another step in us demonstrating what is possible in terms of restoring function in patients who suffer from severe limb injury. It is through collaborative efforts such as this that we are able to make transformational progress in patient care,” says Matthew Carty, a surgeon at Brigham and Women’s Hospital and associate professor at Harvard Medical School, who is also an author of the paper.
Enabling neural control by the person using the limb is a step toward Herr’s lab’s goal of “rebuilding human bodies,” rather than having people rely on ever more sophisticated robotic controllers and sensors — tools that are powerful but do not feel like part of the user’s body.
“The problem with that long-term approach is that the user would never feel embodied with their prosthesis. They would never view the prosthesis as part of their body, part of self,” Herr says. “The approach we’re taking is trying to comprehensively connect the brain of the human to the electromechanics.”
Funding: The research was funded by the MIT K. Lisa Yang Center for Bionics and the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
About this neurotech research news
Author: Anne Trafton
Source: MIT
Contact: Anne Traftn – MIT
Image: The image is credited to Hugh Herr and Hyungeun Song
Original Research: Open access.
“Continuous neural control of a bionic limb restores biomimetic gait after amputation” by Hugh Herr et al. Nature Medicine
Abstract
Continuous neural control of a bionic limb restores biomimetic gait after amputation
For centuries scientists and technologists have sought artificial leg replacements that fully capture the versatility of their intact biological counterparts. However, biological gait requires coordinated volitional and reflexive motor control by complex afferent and efferent neural interplay, making its neuroprosthetic emulation challenging after limb amputation.
Here we hypothesize that continuous neural control of a bionic limb can restore biomimetic gait after below-knee amputation when residual muscle afferents are augmented.
To test this hypothesis, we present a neuroprosthetic interface consisting of surgically connected, agonist–antagonist muscles including muscle-sensing electrodes. In a cohort of seven leg amputees, the interface is shown to augment residual muscle afferents by 18% of biologically intact values.
Compared with a matched amputee cohort without the afferent augmentation, the maximum neuroprosthetic walking speed is increased by 41%, enabling equivalent peak speeds to persons without leg amputation.
Further, this level of afferent augmentation enables biomimetic adaptation to various walking speeds and real-world environments, including slopes, stairs and obstructed pathways.
Our results suggest that even a small augmentation of residual muscle afferents restores biomimetic gait under continuous neuromodulation in individuals with leg amputation.