Summary: The epigenetic histone mutation H3.1K27M works in combination with ACVR1 mutations to cause diffuse intrinsic pontine glioma tumors to form and grow quickly.
Source: Feinberg School of Medicine
A new Northwestern Medicine study finds that a combination of two mutations cause a form of pediatric brain tumors to become more deadly, according to findings published in Nature Communications.
An experimental drug targeting one mutation prolonged survival in models of diffuse intrinsic pontine glioma (DIPG), but questions remain about the drug’s efficacy, according to Oren Becher, MD, associate professor of Pediatrics in the Division of Hematology, Oncology and Stem Cell Transplantation, and senior author of the study. Nevertheless, both mutations are promising targets for future therapies, Becher said.
“About 25 percent of kids with DIPG have these mutations — the mutations must be important for the biology of the disease,” said Becher, who is also an associate professor of Biochemistry and Molecular Genetics and a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. “The first generation inhibitors need to be fine-tuned, but the results of this study show they have the potential to treat this disease in the future.”
Scientists have known about ACVR1 mutations’ role in non-cancerous disease for some time — specifically, in a rare condition called fibrodysplasia ossificans progressiva (FOP). In FOP, muscle and connective tissue such as ligaments and tendons are gradually replaced by bone, causing a progressive loss of mobility for afflicted patients.
During his time at Duke University School of Medicine, Becher and other scientists noticed a surprising number of DIPG patients with similar mutations, leading to a series of studies published in 2014 that demonstrated ACVR1 mutations’ importance in the development of DIPG.
DIPG is a particularly deadly childhood brain tumor, comprising 20 percent of all pediatric brain cancers, and improving therapy has proven difficult over the years, Becher explained.
“The standard of care for the last 50 years has been focal radiation,” Becher said. “50 years of clinical trials have all been negative: we’ve not been able to identify a single drug that can prolong survival in this disease.”
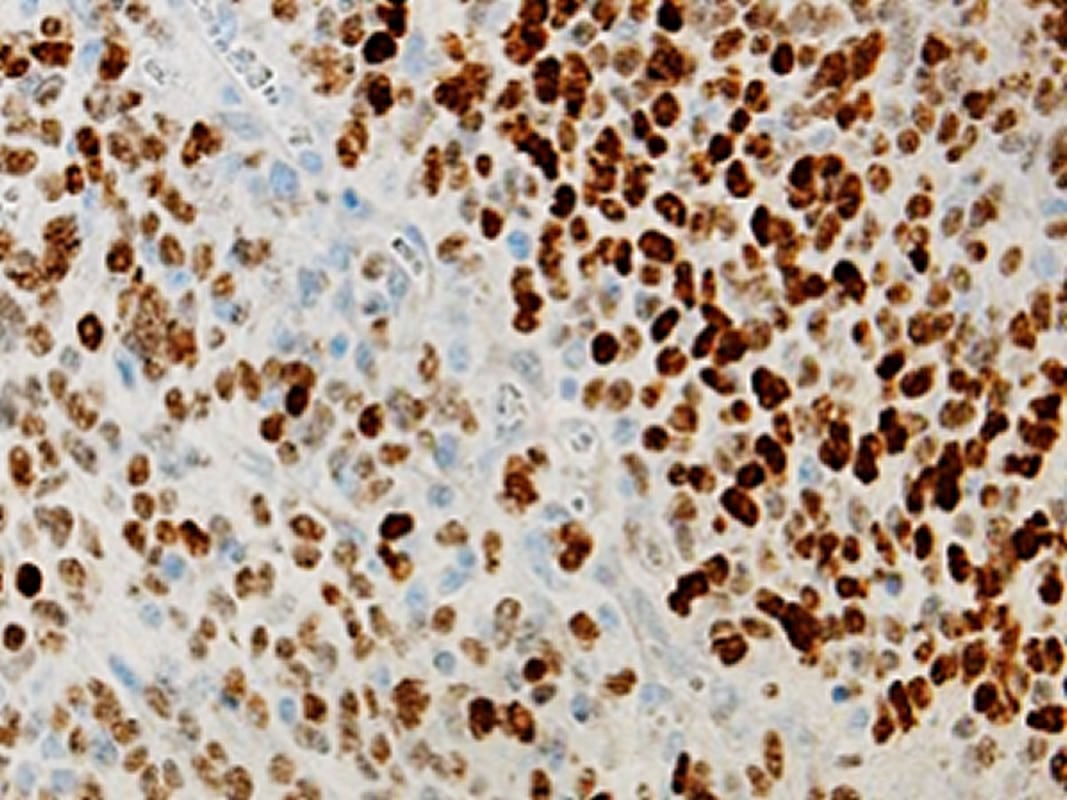
In the current study, Becher and his colleagues used a new model of DIPG to show that ACVR1 mutations aren’t working alone: an epigenetic histone mutation, called H3.1K27M, works in concert with ACVR1 mutations to cause tumors to form and grow more quickly.
While the ACVR1 mutation activates just a handful of genes, the histone mutation acts as a powerful multiplier, raising that figure into the thousands.
“The histone mutation is what makes the ACVR1 mutation much more potent,” Becher said. “The mutations really synergize.”
When both mutations are present, the tumors are more vascular; extra blood vessels helping siphon nutrients away from the brain and into the tumor, fueling growth.
In an attempt to curb this extra growth, Becher and his colleagues explored an experimental ACVR1 inhibitor originally intended to treat FOP, finding it prolonged survival in mouse models of DIPG. However, they discovered that DIPG without mutated ACVR1 also responded well to the drug, indicating the inhibitor may be targeting other molecules or that non-mutant ACVR1 may be involved in cancer.
While promising, the findings underscore how little is known about the mutations, Becher said; he suspects that among the thousands of activated genes lies a pathway that’s making the tumors more vascular — and therefore, a target for inhibition.
“We haven’t figured out which molecules downstream of ACVR1 and the histone mutation are working together to make these blood vessels,” Becher said. “Now we’re trying to find a molecule that we could potentially target or repurpose drugs that already exist. Teasing out which molecules are responsible will get us to a point where we can help these kids.”
Christine Hoeman, PhD, research assistant professor of Pediatrics, was the first author of the study.
Funding: The study was supported by National Institutes of Health grants R01 CA197313 and K02-NS086917, the Damon Runyon Cancer Research Foundation, the Stewart Trust Foundation, Madox’s Warriors, Fly the Kite Foundation, Cristian Rivera Foundation and John McNicholas Pediatric Brain Tumor Foundation.
Source:
Feinberg School of Medicine
Media Contacts:
Will Doss – Feinberg School of Medicine
Image Source:
The image is credited to the researchers.
Original Research: Open access
“ACVR1 R206H cooperates with H3.1K27M in promoting diffuse intrinsic pontine glioma pathogenesis”. Christine M. Hoeman, Francisco J. Cordero, Guo Hu, Katie Misuraca, Megan M. Romero, Herminio J. Cardona, Javad Nazarian, Rintaro Hashizume, Roger McLendon, Paul Yu, Daniele Procissi, Samantha Gadd & Oren J. Becher.
Nature Communications. doi:10.1038/s41467-019-08823-9
Abstract
ACVR1 R206H cooperates with H3.1K27M in promoting diffuse intrinsic pontine glioma pathogenesiss
Diffuse intrinsic pontine glioma (DIPG) is an incurable pediatric brain tumor, with approximately 25% of DIPGs harboring activating ACVR1 mutations that commonly co-associate with H3.1K27M mutations. Here we show that in vitro expression of ACVR1 R206H with and without H3.1K27M upregulates mesenchymal markers and activates Stat3 signaling. In vivo expression of ACVR1 R206H or G328V with H3.1K27M and p53 deletion induces glioma-like lesions but is not sufficient for full gliomagenesis. However, in combination with PDGFA signaling, ACVR1 R206H and H3.1K27M significantly decrease survival and increase tumor incidence. Treatment of ACVR1 R206H mutant DIPGs with exogenous Noggin or the ACVR1 inhibitor LDN212854 significantly prolongs survival, with human ACVR1 mutant DIPG cell lines also being sensitive to LDN212854 treatment. Together, our results demonstrate that ACVR1 R206H and H3.1K27M promote tumor initiation, accelerate gliomagenesis, promote a mesenchymal profile partly due to Stat3 activation, and identify LDN212854 as a promising compound to treat DIPG.






